Chronic diseases, including Type 2 diabetes and various inflammatory disorders, pose a significant challenge to global health, contributing substantially to morbidity and mortality rates. These conditions not only strain healthcare systems but also place a heavy burden on individuals and economies alike, with incidences steadily rising.
Tackling chronic diseases has been complex, primarily due to their multifaceted nature. Unlike conditions caused by single gene mutations, chronic diseases often arise from a confluence of factors. However, groundbreaking research by MIT’s Richard Young and his team, published in Cell on November 27, has identified a potential common factor that might underlie many chronic illnesses: diminished protein mobility.
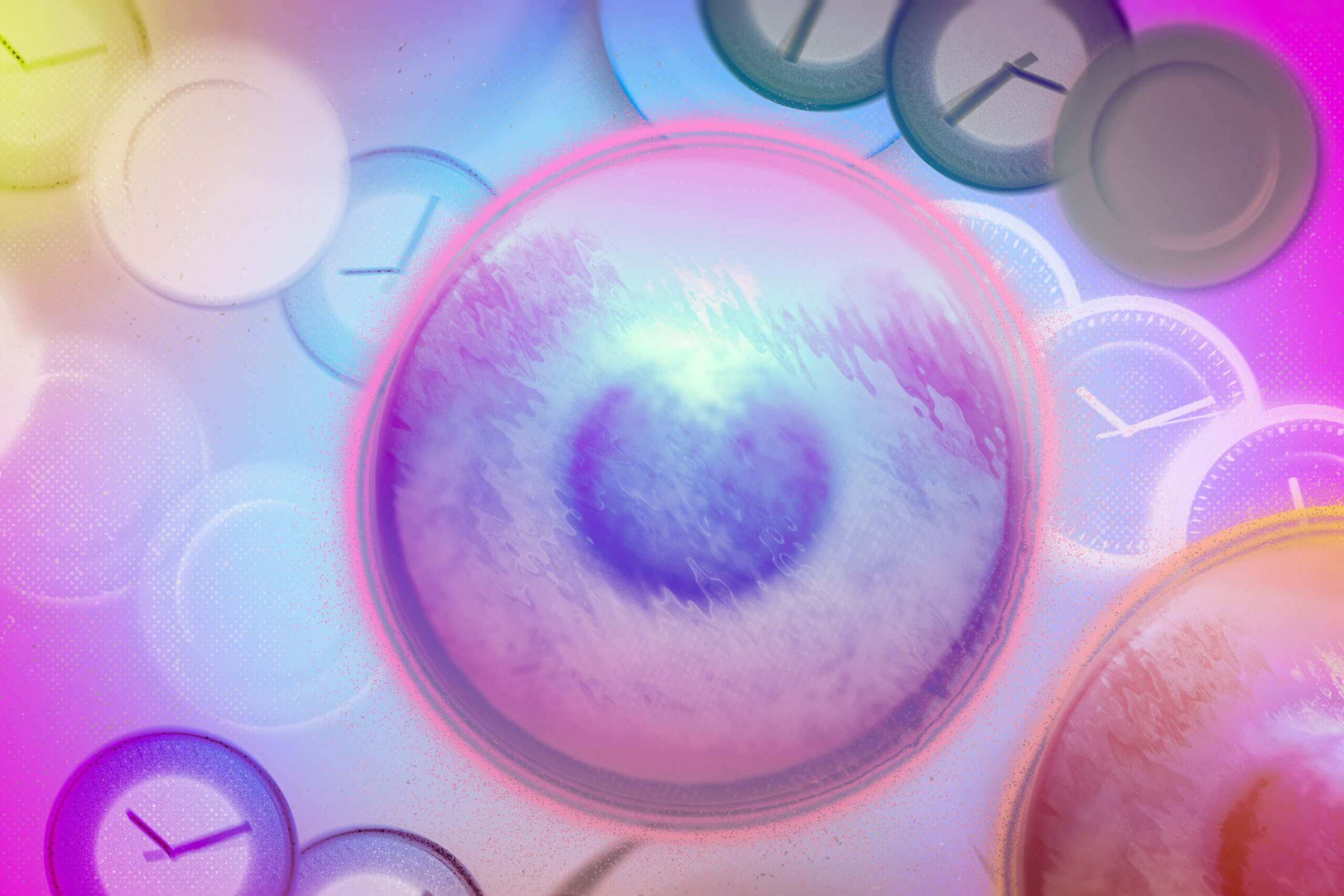
The study reveals that approximately 50% of proteins within cells slow down their movement during chronic disease states, adversely affecting their functions. This discovery positions decreased protein mobility as a pivotal target for novel therapies aimed at restoring cellular functionality in chronic disease contexts.
Young, along with his lab members—including postdoctorate Alessandra Dall’Agnese, graduate students Shannon Moreno and Ming Zheng, and research scientist Tong Ihn Lee—delves into the phenomenon they term ‘proteolethargy.’ Their research elucidates the mechanisms behind this mobility reduction and its implications for cellular dysfunction, proposing exciting new avenues for treatment.
“I’m optimistic about the implications of this work for patients,” remarks Dall’Agnese. “My hope is that we can develop a new class of drugs designed to restore protein mobility, addressing a variety of diseases that share this underlying issue.”
“This research is a testament to the power of interdisciplinary collaboration,” notes Lee. “By integrating expertise from biology, physics, chemistry, computer science, and clinical medicine, we’ve gained new insights into the pathophysiology of chronic disease.”
The Traffic Jam in Cellular Function
So, how does slowed protein movement cause broad cellular dysfunction? Imagine a city where proteins act as diligent workers commuting through a complex, traffic-heavy environment. When proteins move swiftly, they efficiently reach their destinations and accomplish vital tasks. Conversely, if traffic jams occur throughout the city, it leads to delayed operations, postponed activities, and unmet needs.
The slowdown in protein mobility mirrors this scenario in cells impacted by chronic diseases. Proteins normally dart around, interacting with various molecules to execute their functions. When these proteins experience slowdowns, they struggle to reach their molecular counterparts, leading to diminished cellular performance. Young and his colleagues demonstrated that these mobility reductions correspond to significant declines in protein functionality, triggering various issues commonly observed in chronic disease states.
Identifying the Protein Mobility Challenge
The team initially suspected a link between chronic diseases and protein mobility by observing insulin receptor behavior—a key protein that manages cellular sugar uptake in response to insulin. Their earlier work, published in Nature Communications in 2022, hinted that impaired insulin receptor mobility might contribute to diabetes-related complications.
Inspired by the altered cellular responses prevalent in diabetes, the researchers broadened their investigation to a variety of proteins governing vital functions—such as MED1 (gene expression), HP1α (gene silencing), FIB1 (ribosome production), and SRSF2 (messenger RNA splicing). Using advanced tracking techniques, they discovered that most proteins exhibited reduced mobility (approximately 20-35% slower) in disease-affected cells.
“This research exemplifies how physics-based methodologies can illuminate biological processes, particularly in disease contexts,” adds Zheng. “We’ve established a connection between protein movement and disease pathology.”
Moreno adds, “Traditionally, the focus has been on static pictures of proteins or DNA sequences when diagnosing diseases. Our findings reveal that dynamic changes in molecular behavior are equally critical.”
Stuck in Traffic: The Impact of Oxidative Stress
To further unravel what causes proteins to slow down, the researchers examined oxidative stress, identified by elevated levels of reactive oxygen species (ROS) in cells. Known triggers of chronic diseases—like elevated sugar, fat levels, toxins, and inflammatory signals—are linked to increased ROS levels, which disrupt protein interactions. Indeed, when assessing mobility in cells with high ROS levels but no other underlying disease state, comparable mobility issues were noted, implicating oxidative stress as a primary factor.
A crucial distinction emerged: SRSF2 did not experience reduced mobility. The researchers found that this protein lacked surface cysteines—amino acids particularly vulnerable to ROS interference. The formation of bonds between cysteines in different proteins can immobilize them, stalling their functional efficacy. With nearly half of cellular proteins containing surface cysteines, this discovery elucidates the extensive ripple effects on numerous pathways crucial for cellular function, shedding light on the multifaceted nature of chronic diseases.
From Discovery to Potential Treatments
Understanding that oxidative stress-induced decreased protein mobility could drive chronic disease symptoms opens pathways for therapeutic development. In preliminary experiments, cells treated with N-acetyl cysteine—an antioxidant—showed improved protein mobility, suggesting potential avenues for restoring cellular functionality.
The research team is committed to identifying drugs that effectively mitigate ROS levels and enhance protein mobility. They are currently refining assays to screen potential treatments, with a keen eye on additional diseases linked to protein mobility issues and exploring the possible connections to aging processes.
“The intricate biology surrounding chronic diseases has long challenged drug development. Uncovering the shared characteristic of proteolethargy across various diseases presents a unique opportunity to create targeted therapies capable of addressing the broader spectrum of chronic conditions,” concludes Young.
Photo credit & article inspired by: Massachusetts Institute of Technology