Tumors continuously release fragments of DNA from dying cells, which temporarily circulate in a patient’s bloodstream before being rapidly degraded. Many companies have developed blood tests to detect this circulating tumor DNA, aiding in cancer diagnosis, monitoring, and treatment selection.
However, the quantity of tumor DNA present at any given moment is remarkably low, making it difficult to create sufficiently sensitive tests. A collaborative research effort from MIT and the Broad Institute of MIT and Harvard has led to a breakthrough method to significantly enhance the detection of this elusive signal by temporarily hindering the body’s removal of circulating tumor DNA.
The research team has introduced two innovative injectable compounds known as “priming agents.” These agents transiently disrupt the biological processes that eliminate circulating tumor DNA from the bloodstream. In studies conducted on mice, this approach increased the detection rate of early-stage lung metastases from less than 10% to over 75%.
This technique not only promises earlier cancer diagnoses but also allows for more precise identification of tumor mutations, which can guide treatment decisions while enhancing the ability to detect cancer recurrences.
“Administering one of these agents just an hour before a blood draw makes previously invisible signals detectable. The implication is significant: we can provide healthcare professionals conducting liquid biopsies with a more abundant supply of tumor DNA to analyze,” explains Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology at MIT, affiliated with MIT’s Koch Institute for Integrative Cancer Research and the Institute for Medical Engineering and Science.
Bhatia shares authorship of this pioneering study with J. Christopher Love, the Raymond A. and Helen E. St. Laurent Professor of Chemical Engineering at MIT, and Viktor Adalsteinsson, director of the Gerstner Center for Cancer Diagnostics at the Broad Institute.
The lead authors of the published paper in Science include Carmen Martin-Alonso PhD ’23, MIT and Broad Institute postdoc Shervin Tabrizi, and Broad Institute scientist Kan Xiong.
Revolutionizing Liquid Biopsies
Liquid biopsies, which facilitate the detection of small DNA quantities in blood samples, are currently utilized to identify mutations in cancer patients, thus guiding their treatment plans. However, with increased sensitivity, these tests could benefit a significantly larger patient population. Most advancements in liquid biopsy sensitivity have centered on developing next-generation sequencing technologies applied post-sampling.
While contemplating improved methods for liquid biopsies, Bhatia, Love, Adalsteinsson, and their colleagues proposed the idea of enhancing the amount of DNA present in the bloodstream prior to sample collection.
“Tumors persistently generate new cell-free DNA, which serves as the detection signal during blood draws. Yet, existing liquid biopsy technologies are constrained by the limited volume of blood sampled,” comments Love. “Our research shifts the paradigm by introducing an agent that boosts the signal available for collection without requiring increased sample volume.”
The body employs two main mechanisms to eliminate circulating DNA from the bloodstream. First, enzymes known as DNases break down the encountered DNA, while immune cells, specifically macrophages, consume cell-free DNA during liver filtration.
The researchers opted to target each of these elimination processes. To counteract DNase degradation, they engineered a monoclonal antibody designed to attach to circulating DNA, effectively shielding it from enzymatic breakdown.
“Antibodies are widely recognized and safe biopharmaceutical agents across various diseases, including cancer and autoimmune disorders,” Love remarks. “The goal was to utilize this antibody to provide temporary protection to circulating DNA, thereby ensuring that the tumor synthesizes DNA slightly faster than it is being degraded, increasing the blood sample’s concentration.”
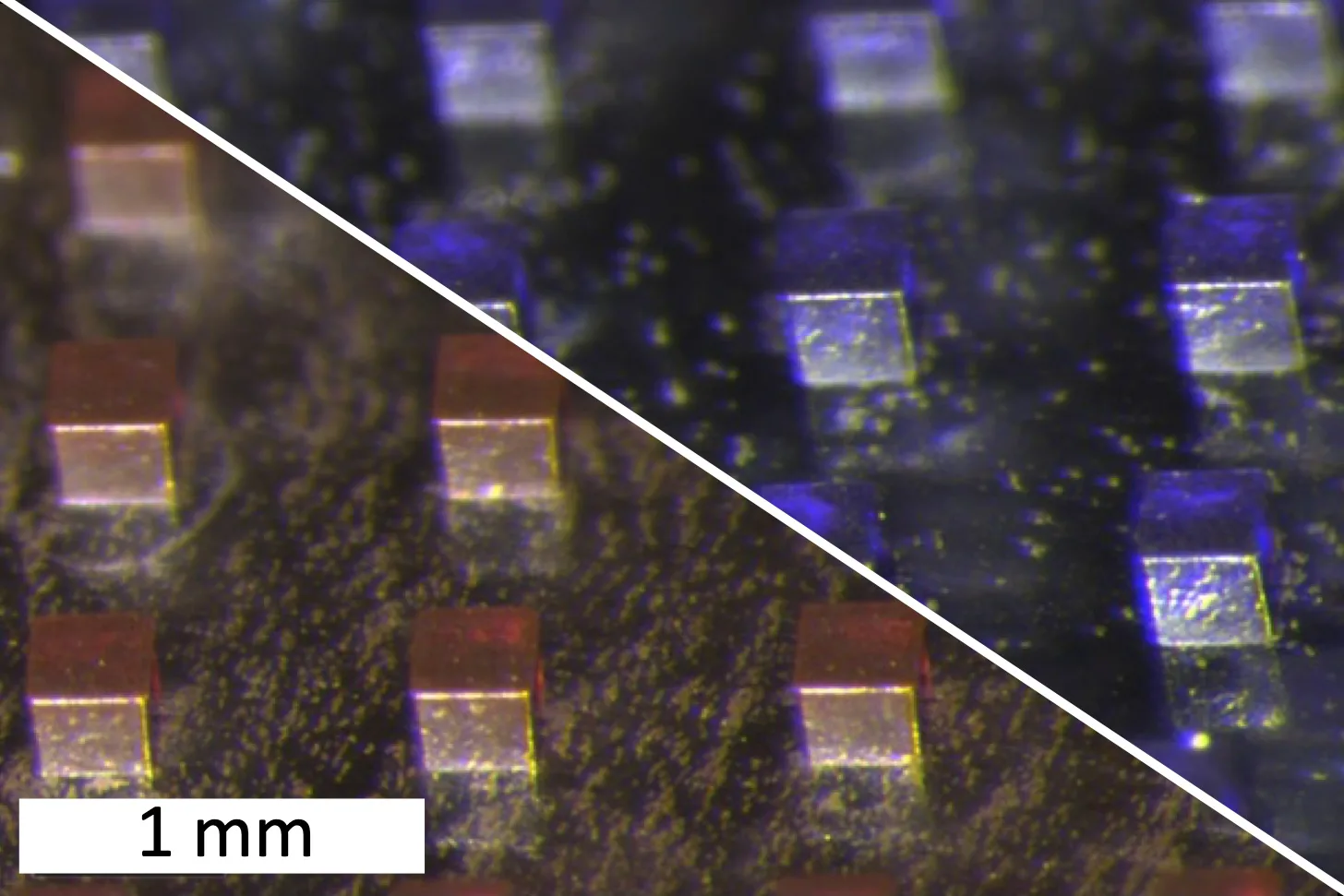
The second priming agent developed is a nanoparticle that obstructs macrophages from ingesting cell-free DNA. Macrophages are known to readily absorb synthetic nanoparticles.
“Considering that DNA behaves as a biological nanoparticle, we surmised that liver macrophages likely consume it in a similar manner to synthetic particles. We validated this hypothesis and proceeded to employ a harmless dummy nanoparticle to occupy these immune cells, allowing the circulating DNA to remain at higher concentrations,” Bhatia adds.
Enhancing Early Tumor Detection
Testing these priming agents on mice with transplanted lung tumor cells demonstrated remarkable results; after two weeks, the injected priming agents resulted in up to a 60-fold increase in circulating tumor DNA recovery in blood samples.
Once the blood samples are collected, they undergo the standard sequencing tests commonly used for liquid biopsy assessments. These tests can effectively identify the tumor DNA, facilitating the precise determination of tumor types and appropriate treatment options.
Moreover, the priming agents present promising prospects for early cancer detection. Researchers found that administering a nanoparticle priming agent prior to blood sampling allowed detection of circulating tumor DNA in 75% of the mice with minimal cancer presence, a noteworthy improvement as none were detectable without this enhancement.
“One of the primary challenges with liquid biopsy testing lies in the scarcity of circulating tumor DNA in samples,” observes Adalsteinsson. “Witnessing the magnitude of our impact thus far is inspiring, as it highlights the potential benefits for patients.”
The effects of the priming agents last for approximately one to two hours, after which DNA levels in the bloodstream return to normal within 24 hours.
“Because these agents reach peak effectiveness swiftly, it allows for patients to receive treatment in a clinical setting, collect blood samples on the same visit,” explains Love. “This rapid clearance is a promising feature for clinical application of this concept.”
The researchers have founded a new company named Amplifyer Bio to focus on further developing this innovative technology, with aspirations of advancing to clinical trials.
“A blood sample is a more accessible diagnostic tool compared to more invasive methods like colonoscopies or mammograms,” states Bhatia. “If these new tools prove predictive, we could usher in a wave of patients who might benefit from early intervention or optimized therapies.”
The research received funding from various esteemed institutions, including the Koch Institute Support Grant from the National Cancer Institute, the Marble Center for Cancer Nanomedicine, and the Bridge Project, a joint initiative between the Koch Institute and the Dana-Farber/Harvard Cancer Center.
Photo credit & article inspired by: Massachusetts Institute of Technology