Have you ever imagined if training your immune system to target cancer cells could be as straightforward as getting it ready to fight Covid-19? Many experts believe that the technology that powered some Covid-19 vaccines—messenger RNA (mRNA)—may hold significant potential in triggering immune responses against cancer.
However, harnessing mRNA to ensure that the immune system launches a sustained and focused assault on cancer cells while sparing healthy cells has been a daunting task.
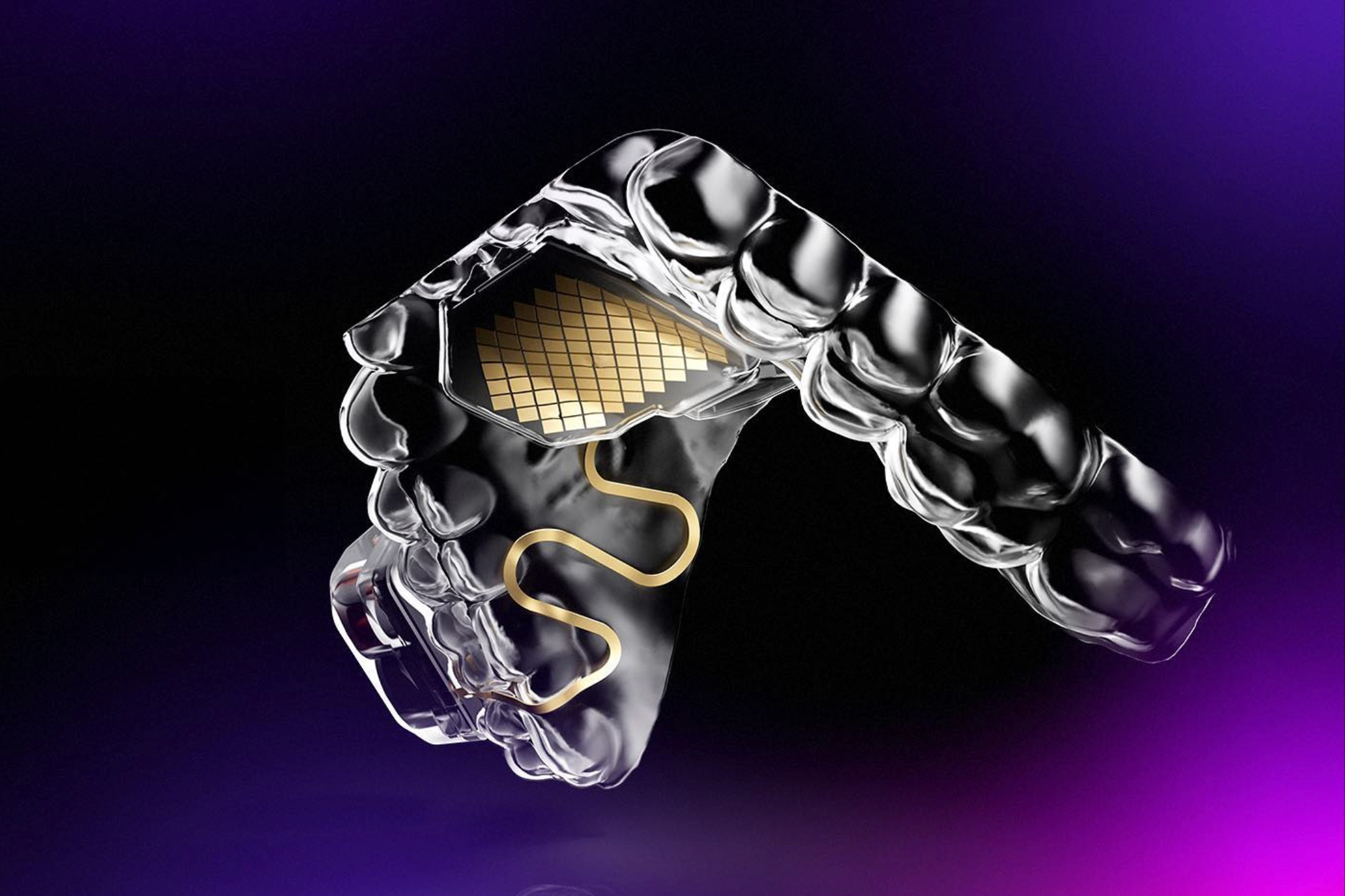
The innovative MIT spinout, Strand Therapeutics, is tackling this challenge with a novel class of mRNA molecules specifically crafted to recognize the types of cells they encounter within the body and to activate therapeutic proteins only upon entering diseased cells.
According to Strand CEO Jacob Becraft, PhD ’19, “Our goal revolves around optimizing the signal-to-noise ratio, with the ‘signal’ being the expression in targeted tissues and the ‘noise’ being the expression in non-target tissues. Our technology enhances the signal to generate more protein expression and prolongs its presence while significantly reducing off-target effects.”
Set to embark on its inaugural clinical trial in April, Strand is testing a self-replicating mRNA molecule designed to relay immune signals from tumors, stimulating the immune system to directly target and eliminate tumor cells. This approach may also enhance existing treatments for various solid tumors.
As the team at Strand pursues the commercialization of their early-stage innovations, they are continually enhancing the capabilities of their “programmable medicines”—refining the mRNA molecules’ capacity to assess their surroundings and produce robust, targeted responses exactly where they’re necessary.
“Self-replicating mRNA was our cornerstone development during our time at MIT and in Strand’s early years,” Becraft reflects. “Now, we’ve expanded into circular mRNAs, enabling each mRNA molecule to produce proteins for extended durations—potentially for weeks. With our growing cell-type specific datasets, we are better equipped to differentiate cell types, allowing our molecules to be targeted with increased safety at higher doses, resulting in more effective treatments.”
Enhancing mRNA Functionality
Becraft’s connection with MIT started when he interned at the lab of Professor Bob Langer during his undergraduate studies at the University of Illinois.
“That experience sparked my understanding of how lab research could translate into startup ventures,” Becraft recalls.
Motivated by this insight, Becraft returned to MIT to pursue his PhD, working alongside Professor Ron Weiss in the Synthetic Biology Center. Here, he collaborated with postdoc Tasuku Kitada to develop genetic “switches” that could regulate protein expression in cells.
Recognizing their research as the foundation for a potential startup, they started exploring this avenue around 2017, utilizing resources from the Martin Trust Center for MIT Entrepreneurship and the MIT Sandbox. Eventually, they collaborated with the Technology Licensing Office to establish Strand’s foundational intellectual property.
“Our initial question was, what’s the greatest unmet need that would help us validate our technology? We swiftly identified oncology as a prime target,” Becraft states.
Researchers have been delving into cancer immunotherapy—harnessing a patient’s immune system to combat cancer— for decades. Notably, some drugs have showcased impressive outcomes, particularly in patients with aggressive, late-stage cancers. Nevertheless, many next-gen cancer immunotherapies hinge on recombinant proteins that are challenging to direct to specific targets and fail to maintain long-term effectiveness.
In recent times, companies like Moderna—which was co-founded by MIT alumni—have advanced the application of mRNAs to produce proteins within cells. Yet, these early mRNA formulations have yet to adapt their activity based on the cells they infiltrate and typically exhibit a short lifespan in the body.
“For optimal engagement of the immune system with a tumor cell, the mRNA must express from the tumor cell itself sustainably,” Becraft explains. “These hurdles have been significant with first-generation mRNA technologies.”
Strand has pioneered what it claims is the world’s first mRNA programming language, giving the company the capability to dictate the specific tissues where their mRNAs express proteins.
“We developed a comprehensive database detailing various cells that could be targeted by the mRNA alongside their microRNA signatures. Using computational tools and machine learning, we can effectively distinguish cell types,” Becraft elaborates. “For example, the mRNA needs to deactivate within liver cells and activate in tumor cells or T-cells.”
Additionally, they leverage self-replicating mRNA techniques to yield more persistent protein expression and immune responses.
“The initial mRNA therapeutics, like the Covid-19 vaccines, mirror how natural mRNAs operate within our bodies,” Becraft distinguishes. “Typically, natural mRNAs only last a few days and produce one type of protein without contextual actions. This feature is ideal for a vaccine, but limiting when aiming to activate a protracted biological process, such as sparking an immune response against a tumor over days or weeks.”
Broad Potential of the Technology
Strand’s first clinical trial will focus on treating solid tumors such as melanoma and triple-negative breast cancer, with plans to expand mRNA therapies for blood cancers as well.
“As we continue to mitigate risk in our scientific translation and innovate new technologies, we plan to broaden our scope,” Becraft notes.
Strand is poised to partner with major pharmaceutical companies and investors to further the advancement of their drug development endeavors. Looking ahead, the founders envision that their mRNA therapies could address a diverse array of diseases.
“Our core thesis is to facilitate amplified expression in specifically programmed target cells over extended periods,” Becraft concludes. “This strategy can enhance various applications, including immunotherapies like CAR T-cell therapy for both cancer patients and those with autoimmune disorders, as well as address conditions requiring targeted delivery and protein expression across different diseases.”
Photo credit & article inspired by: Massachusetts Institute of Technology