The ancient Greek philosopher Aristotle once posited that the human heart was tri-chambered and deemed it the most crucial organ for governing motion, sensation, and thought. Fast forward to today, we recognize that the human heart actually has four chambers, while the brain predominantly oversees these functions. Nevertheless, Aristotle’s assertion about the heart’s importance remains valid; it effectively pumps blood and essential nutrients throughout the body. When faced with a perilous condition like heart failure, the heart’s ability to nourish other organs diminishes significantly.
A team of researchers from MIT and Harvard Medical School recently unveiled a groundbreaking open-access paper in Nature Communications Medicine, presenting a noninvasive deep learning method that processes electrocardiogram (ECG) signals to predict heart failure risk with remarkable accuracy. During clinical trials, this innovative model exhibited results comparable to traditional invasive methods, sparking hope for those susceptible to heart failure—a condition that has alarmingly surged in mortality rates, particularly among young adults, largely attributable to rising obesity and diabetes rates.
“This research embodies concepts I’ve discussed for years,” shares Collin Stultz, the paper’s senior author and director of the Harvard-MIT Program in Health Sciences and Technology. He is also an affiliate of the MIT Abdul Latif Jameel Clinic for Machine Learning in Health. “Our goal is to identify individuals in the early stages of illness, allowing timely interventions to prevent hospitalizations.”
The heart consists of four chambers: two atria and two ventricles, with the right side comprising one atrium and one ventricle, and the left side similarly structured. In a healthy heart, these chambers function synchronously: oxygen-poor blood enters the right atrium, which contracts to push it into the right ventricle—subsequently directing it to the lungs for oxygenation. The oxygen-rich blood then flows into the left atrium, is pumped into the left ventricle, and finally ejected from the aorta, circulating throughout the body.
Stultz elaborates, “When pressures in the left atrium begin to rise, the drainage of blood from the lungs can become obstructed due to the elevated pressure. Higher left atrial pressure correlates with increased pulmonary symptoms, like shortness of breath.” Alongside his role as a professor of electrical engineering and computer science, Stultz practices cardiology at Mass General Hospital (MGH).
Traditionally, right heart catheterization (RHC) serves as the gold standard for measuring left atrial pressure. This invasive technique entails the insertion of a catheter connected to a pressure transmitter within the right heart and pulmonary arteries. Before resorting to RHC, doctors often prefer noninvasive assessments based on patient weight, blood pressure, and heart rate.
However, Stultz argues that these conventional estimates are oftentimes rough indicators. Research indicates that approximately 25% of heart failure patients are readmitted within 30 days due to insufficient monitoring. “We are pursuing a method that reveals intimate insights similar to an invasive device, without the discomfort of a simple weight scale,” he asserts.
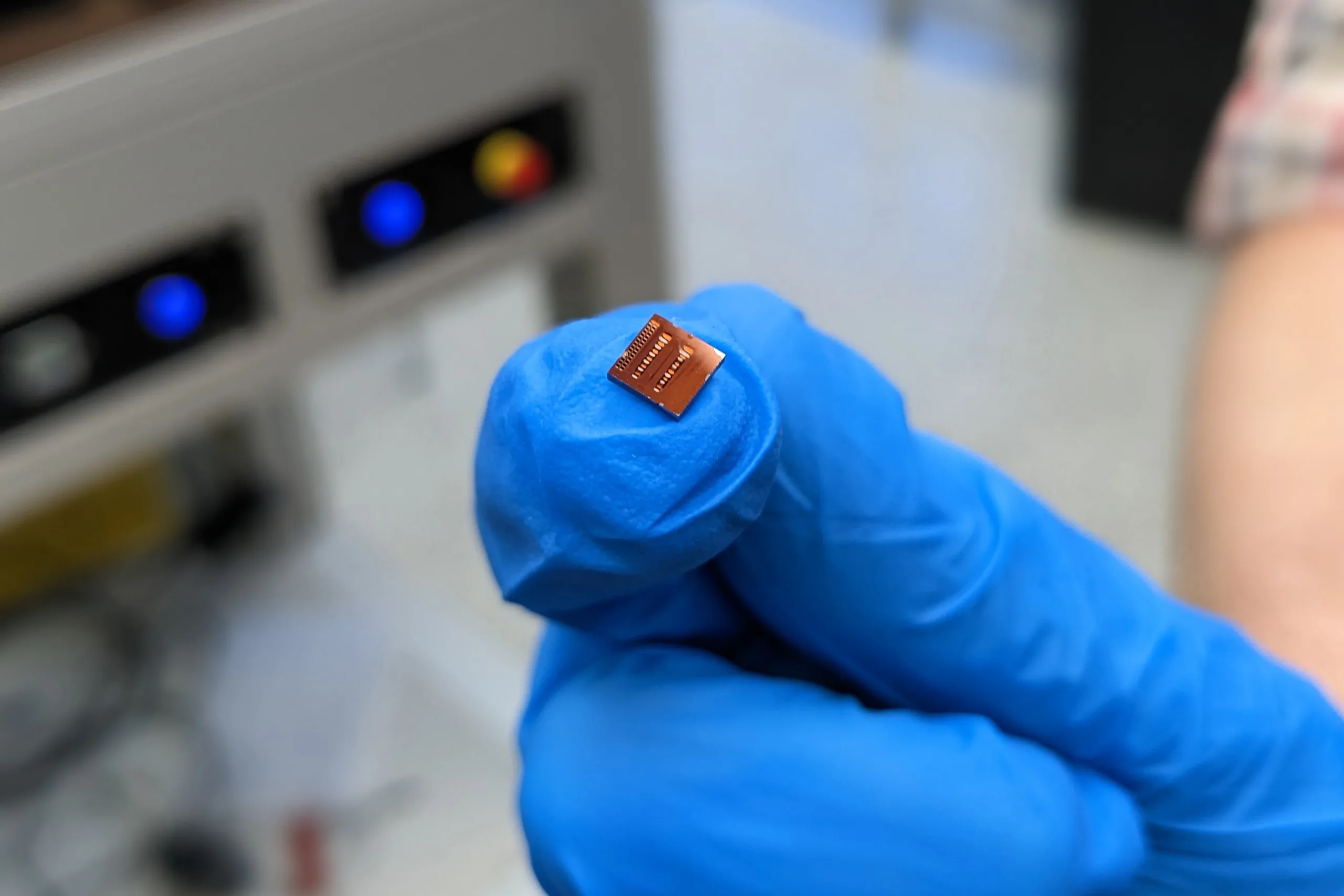
Typically, a 12-lead ECG, which requires 10 adhesive patches on the patient, delivers multi-angle insights into cardiac condition. However, accessibility to 12-lead machines is limited to clinical settings, and their use for heart failure risk assessment is minimal.
This is where Stultz and his team introduce the Cardiac Hemodynamic AI monitoring System (CHAIS)—a deep neural network devised to analyze ECG data from a solitary lead. This means that patients can wear a single, commercially available adhesive patch on their chest, liberating them from the constraints of clinical equipment.
To evaluate CHAIS against the current standard of RHC, researchers selected patients already scheduled for catheterization. Participants were asked to don the patch for 24 to 48 hours before the procedure, though they were required to remove it prior to catheterization. “Remarkably, the predictive accuracy was 0.875 within an hour and a half before the procedure,” Stultz highlights. “Thus, data from the device can provide insights comparable to those from immediate catheterization.”
“Every cardiologist appreciates the significance of left atrial pressure in assessing cardiac function and refining treatment approaches for heart failure patients,” states Aaron Aguirre SM ’03, PhD ’08, a cardiologist at MGH. “This research is crucial as it presents a noninvasive opportunity to estimate a vital clinical measurement with a widely accessible tool.”
Aguirre, who earned his PhD in medical engineering and medical physics at MIT, believes that with further clinical validation, CHAIS will serve two pivotal roles: identifying patients who would benefit from invasive testing via RHC and enabling ongoing monitoring of left atrial pressure in cardiac patients. “A noninvasive tool can crucially enhance treatment strategies, whether patients are at home or in the hospital,” he explains enthusiastically. “I eagerly anticipate the next steps from the MIT team.”
The advantages extend beyond patient care—managing complex heart failure cases poses challenges in preventing readmissions without resorting to permanent implants, which would further strain an already overworked medical workforce.
The research team is currently involved in another clinical trial using CHAIS at MGH and Boston Medical Center, with hopes of completing it soon for data analysis.
“In my opinion, the true potential of AI in healthcare lies in delivering equitable, high-quality care to all individuals, irrespective of socioeconomic factors,” asserts Stultz. “This study brings us one step closer to achieving that vision.”
Photo credit & article inspired by: Massachusetts Institute of Technology