Patients battling late-stage cancer often face the daunting challenge of enduring several treatment rounds, which may lead to unwanted side effects and aren’t always effective. To broaden the treatment landscape for these patients, researchers at MIT have developed innovative tiny particles that can be implanted directly at the tumor site, delivering a dual-action approach combining heat and chemotherapy.
This groundbreaking method aims to sidestep the usual side effects associated with intravenous chemotherapy. By merging the two therapies, the researchers believe that the treatment could enhance the patient’s lifespan more effectively than administering therapies separately. In a study conducted on mice, this dual therapy approach resulted in the complete eradication of tumors in most subjects and significantly increased their survival rates.
“This technology could be particularly valuable in managing rapidly growing tumors,” states Ana Jaklenec, principal investigator at MIT’s Koch Institute for Integrative Cancer Research. “Our objective is to help patients who have limited options, potentially extending their life or improving their quality of life during treatment.”
Jaklenec co-authored the study alongside Angela Belcher, Professor of Biological Engineering and Materials Science, and Robert Langer, an MIT Institute Professor. Maria Kanelli, a former MIT postdoctoral researcher, leads the paper published in ACS Nano.
Innovative Dual Therapy Approach
As patients with advanced tumors often undergo a combination of treatments including chemotherapy, surgery, and radiation, researchers are keen on exploring newer options. One such approach is phototherapy, which uses implanted or injected particles heated by an external laser to reach temperatures sufficient to destroy nearby tumor cells without harming adjacent healthy tissue.
Current clinical trials primarily utilize gold nanoparticles that generate heat when exposed to near-infrared light. The MIT team aimed to develop a method that would allow for concurrent phototherapy and chemotherapy, which they hypothesized could ease the treatment burden on patients while amplifying treatment efficacy through combined effects. They selected a promising inorganic material, molybdenum sulfide, as the phototherapeutic agent due to its efficient heat conversion, which enables the use of lower-powered lasers.
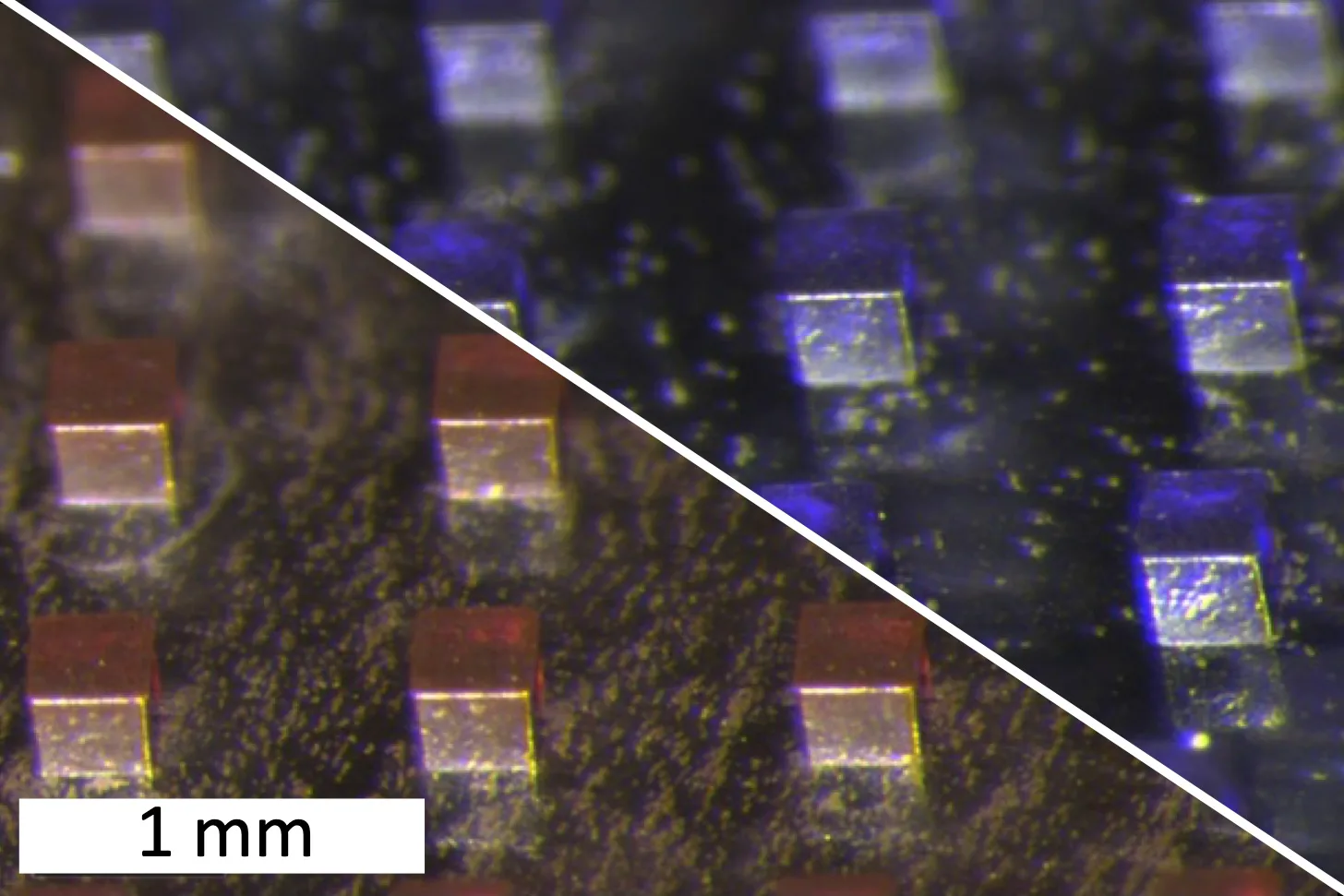
To fabricate a microparticle capable of delivering both therapies, the researchers integrated molybdenum disulfide nanosheets with the chemotherapeutic agents doxorubicin and violacein. The combination was mixed with polycaprolactone, a polymer, and formed into microparticles with various shapes and sizes.
In this study, researchers created cubic particles measuring 200 micrometers on each side. Once injected into the tumor site, these particles remain positioned throughout the treatment cycle. An external near-infrared laser is then applied to heat the particles, targeting tissue at depths ranging from a few millimeters to centimeters.
“The beauty of this platform lies in its capacity for demand-driven activation,” explains Kanelli. “You administer it once via intratumoral injection, and then can activate the platform using an external laser to release the drug while simultaneously achieving thermal ablation of tumor cells.”
To refine their treatment approach, the researchers utilized machine-learning algorithms to optimize the laser power, irradiation time, and phototherapeutic concentration that would yield the most favorable results. They ultimately settled on a treatment cycle lasting approximately three minutes, heating the particles to around 50 degrees Celsius—hot enough to eliminate tumor cells. At this temperature, the polymer matrix within the particles begins to melt, facilitating the release of the encapsulated chemotherapy drug.
“This machine-learning-optimized laser system empowers us to deliver low-dose, localized chemotherapy, leveraging the deep tissue penetration of near-infrared light for a pulsatile and on-demand photothermal therapy. This synergy results in notably lower systemic toxicity compared to traditional chemotherapy treatments,” remarks Neelkanth Bardhan, a research scientist in the Belcher Lab and co-author of the paper.
Effectiveness in Tumor Elimination
The research team tested their microparticle treatment on mice injected with an aggressive strain of cancer cells from triple-negative breast tumors. After tumor formation, roughly 25 microparticles were implanted per tumor, followed by three sessions of laser treatment spaced three days apart.
“This study showcases the potential of near-infrared-responsive material systems in the cancer treatment landscape,” says Belcher, who previously worked on near-infrared imaging systems for diagnosis and treatment in ovarian cancer. “The ability to control drug release at specific intervals with light, following a single particle injection, can transform treatment options into less painful alternatives that may improve patient compliance.”
Mice receiving this innovative treatment exhibited complete tumor eradication and significantly outlived those subjected to solitary chemotherapy, phototherapy, or no treatment at all. Furthermore, mice undergoing all three laser treatments demonstrated remarkable benefits compared to those subjected to only a single laser treatment.
The biocompatible polymer used to manufacture these particles has already received FDA approval for medical applications. The researchers are now looking ahead to testing their particles in larger animal models, with aspirations to eventually conduct clinical trials. They anticipate this treatment could be beneficial for a variety of solid tumors, including metastatic varieties.
This research received funding from the Bodossaki Foundation, the Onassis Foundation, a Mazumdar-Shaw International Oncology Fellowship, a National Cancer Institute Fellowship, and the Koch Institute Support (core) Grant from the National Cancer Institute.
Photo credit & article inspired by: Massachusetts Institute of Technology