Ketamine, recognized as an Essential Medicine by the World Health Organization, has gained prominence for its diverse applications, ranging from sedation and pain management to general anesthesia and its groundbreaking role in treating treatment-resistant depression. Researchers have identified the key targets within brain cells and observed ketamine’s influence on overall brain activity. However, a comprehensive understanding of how these two aspects are interlinked has remained elusive. A recent study conducted by a collaborative team across four Boston institutions leverages computational modeling to shed light on the physiological intricacies, bridging this knowledge gap and unveiling new insights into ketamine’s mechanisms.
Co-senior author Emery N. Brown, an expert in Computational Neuroscience and Medical Engineering from The Picower Institute at MIT, notes, “This modeling work has significantly advanced our understanding of how ketamine alters arousal states and its therapeutic advantages in treating depression.”
The research, conducted by teams from MIT, Boston University (BU), Massachusetts General Hospital (MGH), and Harvard University, presents a model in a study published on May 20 in Proceedings of the National Academy of Sciences. The implications of this model could empower healthcare providers to optimize ketamine’s use in clinical settings.
“Understanding the mechanisms at play when administering ketamine enables physicians to harness its benefits while minimizing potential drawbacks,” explains study lead author Elie Adam, a researcher at MIT slated to join Harvard Medical School’s faculty and establish a lab at MGH. “This insight allows for enhanced management of the drug’s beneficial effects.”
Understanding the Mechanisms
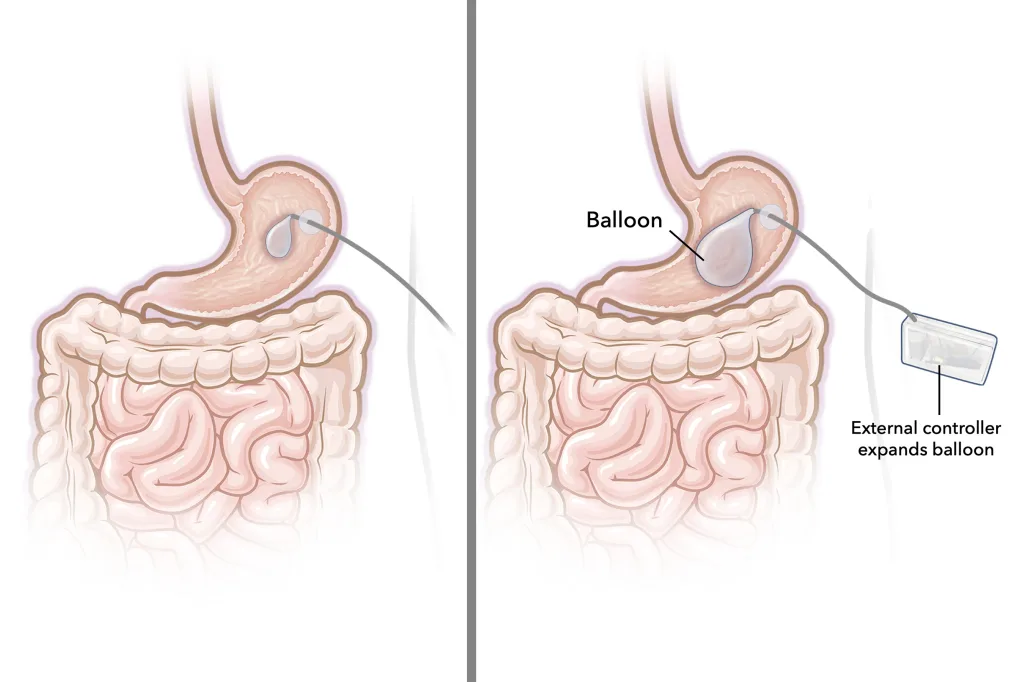
A pivotal advancement in this study involved detailed biophysical modeling of how ketamine interacts with the brain’s NMDA receptors found in the cortex, which is integral for sensory processing and cognition. By blocking these NMDA receptors, ketamine modulates the release of the excitatory neurotransmitter glutamate.
Furthermore, the NMDA channels typically open and close slowly, allowing ions to flow in and out of the neuron, regulating its electrical characteristics. While magnesium can naturally block these channels, ketamine proves to be a more potent inhibitor.
This blocking effect reduces the voltage build-up across neurons, which is essential for triggering electrochemical communication among them. The researchers’ model surpasses earlier ones by illustrating how the blocking and unblocking influences neural activity in a more integrated manner.
“Details often overlooked can be crucial for grasping cognitive functions,” emphasizes co-corresponding author Nancy Kopell, a mathematics professor at BU. “The dynamics at the NMDA receptor level significantly affect network behavior more than previously realized.”
Using their model, the team simulated the impact of various ketamine doses on NMDA receptor activity within a simplified version of the brain’s network. This simulation included diverse neuron types: one excitatory and two inhibitory. It differentiated between “tonic” interneurons that often suppress activity and “phasic” interneurons that respond aggressively to excitatory signals.
The researchers successfully replicated brain wave patterns measured via EEG in human subjects administered different ketamine doses, as well as neural spiking observed in animals. At lower doses, ketamine amplified brain wave power in the fast gamma frequency range (30-40 Hz). Conversely, at higher doses that induce unconsciousness, these gamma waves experienced interruptions marked by “down” states where only slow-frequency delta waves emerged. This intermittent disruption hampers communication across the cortex, leading to a loss of consciousness.
Key Discoveries
The simulations unveiled several crucial mechanisms that account for the observed dynamics. The first finding indicates that ketamine can enhance network activity by inhibiting certain interneurons. When given ketamine, the NMDA receptors’ natural kinetic behavior allows a modest current to flow when neurons are inactive. Many neurons in the network at optimal excitation levels use this current to spontaneously fire. However, with ketamine’s interference, this current diminishes, rendering those neurons inactive. Although ketamine equally affects all neurons, tonic inhibitory ones become suppressed, liberating other excitatory or inhibitory neurons to fire more readily, resulting in ketamine-inducing excitatory brain activity. This heightened excitation facilitates rapid blocking and unblocking of NMDA receptors, leading to bursts of neuronal firing.
Another significant discovery revolves around the synchronization of bursts into gamma frequency waves with ketamine administration. The research revealed that phasic inhibitory interneurons, spurred by glutamate input from excitatory neurons, start spiking and transmitting GABA signals back to the excitatory neurons, effectively dampening their firing. This simultaneous inhibitory action synchronizes the activity of the excitatory neurons, generating well-coordinated gamma brain waves.
“It was surprising to find that an individual synaptic receptor, such as NMDA, can significantly influence gamma oscillations and that these oscillations can impact broader network-level activities,” recounts co-corresponding author Michelle McCarthy, a research assistant professor of mathematics at BU. “This realization emerged from a detailed physiological model of the NMDA receptor, revealing a gamma timing scale not usually attributed to it.”
What about the periodic down states that occur with higher doses of ketamine, which lead to unconsciousness? The simulations indicated that excitatory neurons’ gamma-frequency activity cannot be sustained due to the NMDA receptor kinetics being compromised. Eventually, the excitatory neurons grow fatigued from GABA inhibition exerted by phasic interneurons, resulting in a down state. However, once the excitatory neurons stop releasing glutamate, the phasic cells cease their GABA inhibition, allowing excitatory neurons to recuperate, thus restarting the cycle.
Connecting to Antidepressant Effects
The model also proposes an intriguing connection to ketamine’s antidepressant effects. It suggests that increased gamma activity could promote synchronization among neurons with a peptide called VIP, known for its health-boosting properties, including inflammation reduction that outlasts ketamine’s influence on NMDA receptors. This observation hints that ketamine may possess therapeutic qualities extending beyond its antidepressant capabilities, though the authors acknowledge that this idea requires further experimental validation.
“Recognizing that NMDA receptor specifics can lead to heightened gamma oscillations has paved the way for a new theory regarding ketamine’s role in depression treatment,” states Kopell.
Co-authors of the research include Marek Kowalski, Oluwaseun Akeju, and Earl K. Miller. The study received funding from the JPB Foundation, The Picower Institute for Learning and Memory, The Simons Center for The Social Brain, the National Institutes of Health, and several individual donors.
Photo credit & article inspired by: Massachusetts Institute of Technology