Autosomal dominant polycystic kidney disease (ADPKD) is the most prevalent form of polycystic kidney disease, impacting over 12 million individuals globally. This condition can lead to significant kidney enlargement and eventually kidney failure, leaving many patients reliant on dialysis or a kidney transplant by age 60.
Researchers from MIT and Yale University School of Medicine are excited to reveal that a compound initially developed for cancer treatment shows potential in combating ADPKD. This innovative drug leverages the susceptibility of kidney cyst cells to oxidative stress—an imbalance between damaging free radicals and beneficial antioxidants.
In their study using two distinct mouse models of ADPKD, the researchers observed a dramatic reduction in kidney cyst sizes with no adverse effects on healthy kidney cells.
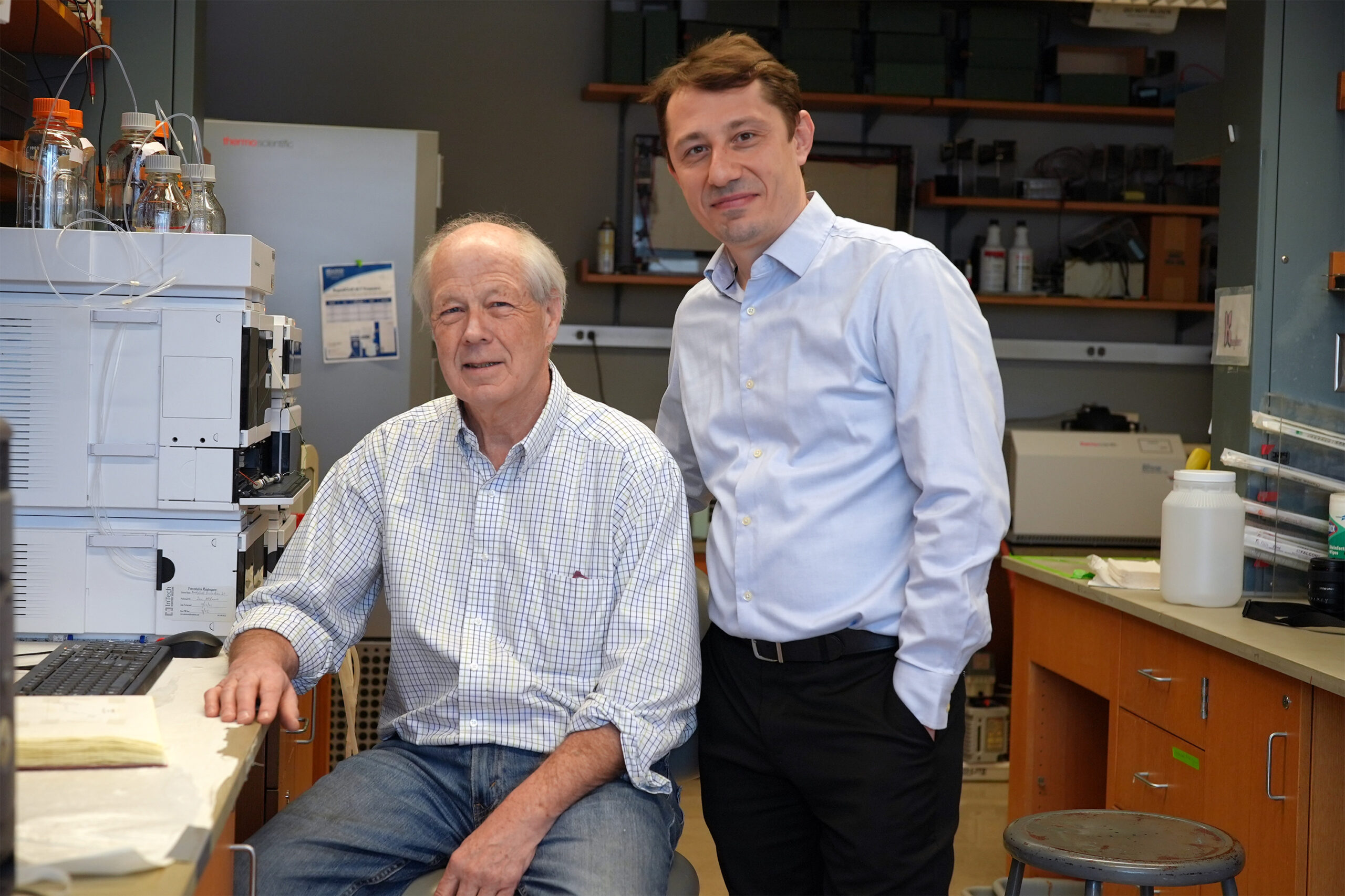
“We genuinely believe this could revolutionize treatment approaches for this critical disease,” stated Bogdan Fedeles, a research scientist and program manager at MIT’s Center for Environmental Health Sciences. He is the lead author of the study published this week in the Proceedings of the National Academy of Sciences.
Senior authors of the paper include John Essigmann, the William R. and Betsy P. Leitch Professor of Biological Engineering and Chemistry at MIT; Sorin Fedeles, executive director of the Polycystic Kidney Disease Outcomes Consortium and assistant professor (adjunct) at Yale University School of Medicine; and Stefan Somlo, the C.N.H. Long Professor of Medicine and Genetics and chief of nephrology at Yale University School of Medicine. For more details, read the full paper here.
Understanding Cells Under Stress
ADPKD often develops gradually, typically diagnosed in patients during their 30s and usually not affecting kidney function significantly until their 60s. Currently, the only FDA-approved treatment, tolvaptan, can slow cyst growth but carries side effects such as frequent urination and potential liver damage.
Essigmann’s lab originally focused on cancer drugs, with the current ADPKD research stemming from nearly 25 years of work. MIT scientist Robert Croy, an author of the new PNAS study, synthesized compounds that contained a DNA-damaging agent called aniline mustard, which targets cancer cells for destruction.
In mid-2000s, as Fedeles was finishing his graduate studies in Essigmann’s lab, they discovered that these compounds, alongside their DNA-damaging properties, also induce oxidative stress by disrupting mitochondrial function—the cells’ energy producers.
Since tumor cells are inherently under oxidative stress due to their abnormal metabolic activity, introducing 11beta compounds exacerbates this condition, leading to increased cell death. Their earlier work showed promising results, including significant suppression of prostate tumor growth in mouse models.
A conversation between Bogdan and Sorin Fedeles sparked curiosity about whether these compounds could similarly treat kidney cysts. Recent findings indicated that kidney cyst cells also experience oxidative stress akin to that in cancer cells due to dysfunctional metabolism.
“It was an intriguing hypothesis that the compounds I was working with could potentially benefit polycystic kidney disease,” said Bogdan Fedeles.
The 11beta compounds hinder cellular processes by disrupting ATP (adenosine triphosphate) production within mitochondria, as well as depleting NADPH, a key antioxidant cofactor. Amidst persistent oxidative stress, kidney cyst cells display lower tolerance levels, leading them to cell death while sparing healthy kidney cells.
Results: Shrinking Kidney Cysts
Utilizing two mouse models of ADPKD, the researchers successfully demonstrated that 11beta-dichloro significantly reduced the size of kidney cysts and enhanced kidney function.
They also developed a safer variant, 11beta-dipropyl, which lacks the DNA-damaging properties and was equally effective in early-onset PKD models. Remarkably, the treatment did not harm healthy kidney cells since they can better withstand slight oxidative stress compared to the affected cystic cells. Furthermore, treatment led to the reduction of biomarkers associated with inflammation and fibrosis.
These promising results imply that, for patients, administering the 11beta compounds periodically—perhaps once a year—could substantially delay disease progression, potentially reducing the reliance on constant therapies like tolvaptan.
“Our understanding of cyst growth suggests that infrequent pulsatile treatment could significantly influence kidney health,” noted Sorin Fedeles.
Looking ahead, the researchers aim to conduct additional tests on 11beta-dipropyl and explore larger-scale production methods. They also intend to investigate other related compounds that could serve as viable drug options for treating PKD.
The collaborative research included contributions from MIT researchers: Nina Gubina, former postdoc Sakunchai Khumsubdee, former postdoc Denise Andrade, and former undergraduates Sally S. Liu ’20 and co-op student Jake Campolo. Funding sources for this research included the PKD Foundation, the U.S. Department of Defense, the National Institutes of Health, and the National Institute of Environmental Health Sciences via MIT’s Center for Environmental Health Sciences.
Photo credit & article inspired by: Massachusetts Institute of Technology