Patients undergoing chemotherapy frequently grapple with cognitive challenges, commonly referred to as “chemo brain.” This condition manifests as memory deficits and trouble concentrating, resulting from the side effects of chemotherapy.
Researchers at MIT have discovered that a noninvasive treatment that triggers gamma frequency brain waves might offer a solution for those affected by chemo brain. In experiments involving mice, daily light and sound therapy at a frequency of 40 hertz demonstrated protective qualities against chemotherapy-induced brain damage. This innovative approach not only prevented memory loss but also improved various cognitive functions.
Originally devised for Alzheimer’s treatment, this method may exert far-reaching benefits across different neurological disorders, according to the researchers.
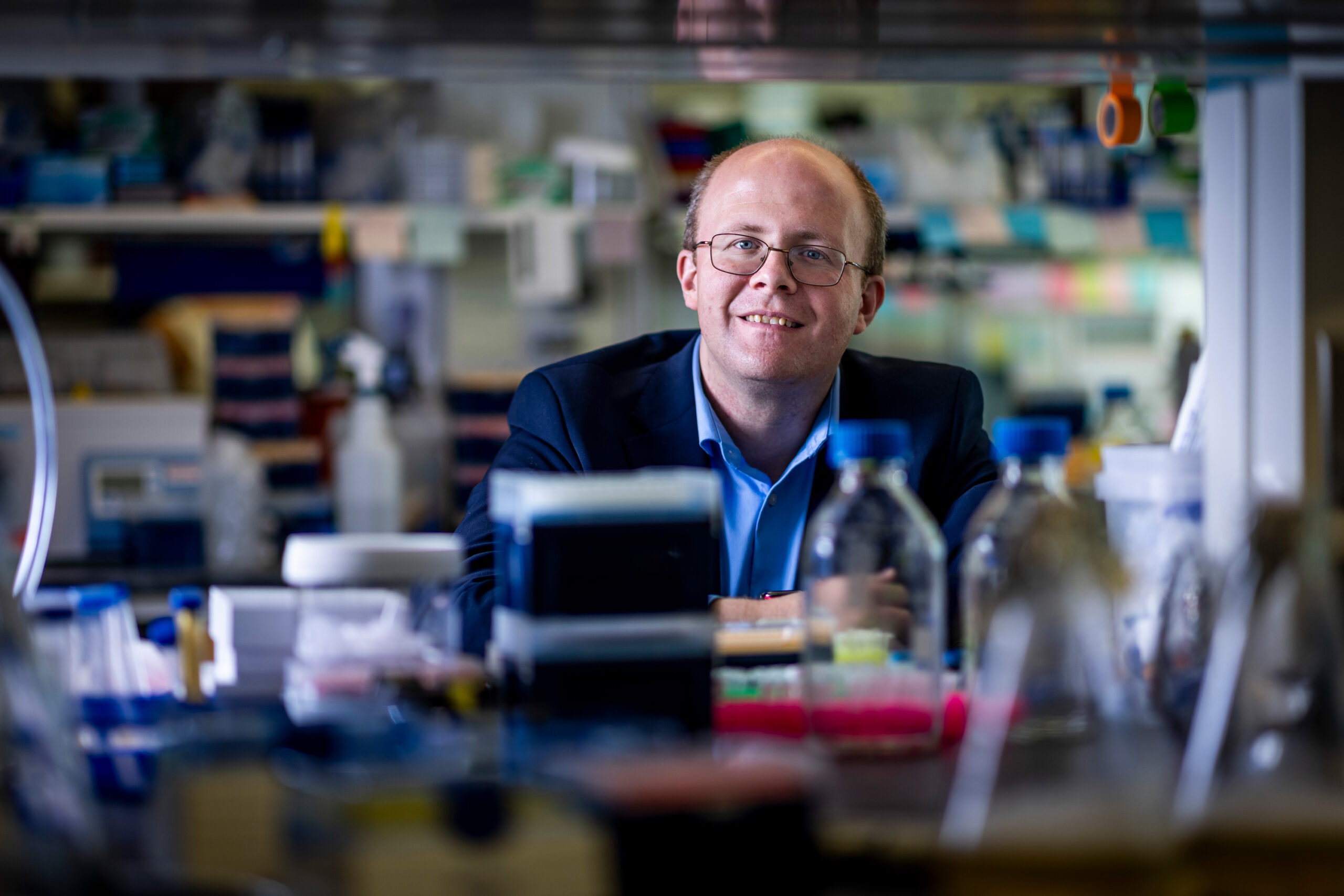
“Our findings reveal that the treatment can diminish DNA damage, lower inflammation, and boost the production of oligodendrocytes, crucial cells responsible for creating the myelin sheath around nerve fibers,” explains Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory. “Additionally, we observed enhanced learning, memory, and executive functions in the animals studied.”
Tsai, who is the senior author of the study, which was published today in Science Translational Medicine, conducted the research alongside lead author TaeHyun Kim, an MIT postdoc.
Understanding Protective Brain Waves
Years ago, Tsai and her team began investigating the effects of light flickering at 40 hertz as a potential intervention for cognitive symptoms in Alzheimer’s patients. Previous studies indicated that those suffering from Alzheimer’s displayed impaired gamma oscillations, whose frequencies range from 25 to 80 hertz and play a vital role in cognitive capabilities such as attention, perception, and memory.
Tsai’s mouse studies revealed that both flickering light and specific sound frequencies (40 hertz) could stimulate gamma waves, offering several protective benefits, including the prevention of amyloid beta plaque formation. Moreover, combining auditory and visual stimuli significantly enhances these protective effects. Encouragingly, early-phase clinical trials have confirmed the safety and neurological benefits of this treatment in individuals with early-stage Alzheimer’s disease.
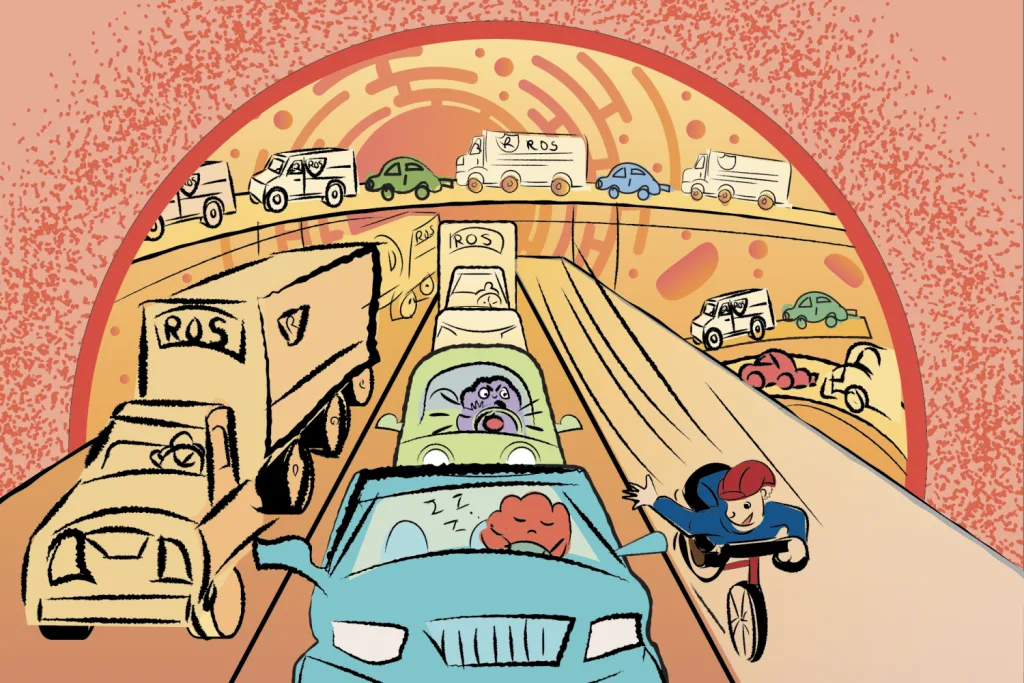
In this recent investigation, the team aimed to explore whether this therapy could mitigate the cognitive impacts of chemotherapy. Research indicates that chemotherapy drugs often induce brain inflammation and other harmful effects, such as white matter loss—the essential networks that facilitate communication between various brain regions. These drugs are also linked to the degradation of myelin, the protective layer enabling efficient neuronal signal propagation. Such damage parallels the neurological effects seen in Alzheimer’s.
“Chemo brain intrigued us due to its widespread prevalence and the extensive research available regarding post-chemotherapy brain health,” Tsai noted. “From previous findings, we know that gamma sensory stimulation can reduce inflammation, prompting us to evaluate its efficacy in the chemo brain model.”
The researchers employed an experimental model using mice treated with cisplatin, a chemotherapy agent commonly used for various cancers, including testicular and ovarian. Mice received cisplatin in cycles of five days on, five days off, while one group received only chemotherapy, and the other group received 40-hertz light and sound therapy daily.
After three weeks, mice treated with cisplatin alone exhibited typical chemotherapy effects: a reduction in brain volume, increased DNA damage, inflammation, and demyelination. Moreover, these mice showed a decline in oligodendrocytes, essential for maintaining myelin production.
In contrast, mice receiving gamma therapy alongside cisplatin demonstrated notable reductions in these adverse effects. Behavioral assessments also revealed that treated mice excelled in memory and executive function tests.
Uncovering Fundamental Mechanisms
Utilizing single-cell RNA sequencing, the research team analyzed gene expression changes in the gamma-treated mice. They discovered that inflammation-related genes and those triggering cell death were notably suppressed, particularly within the oligodendrocytes responsible for myelin synthesis.
Some beneficial effects of gamma treatment persisted in afflicted mice even four months post-treatment, although efficacy waned if therapy began three months after chemotherapy ended.
Importantly, the researchers observed that gamma therapy also alleviated chemo brain symptoms in mice treated with methotrexate, another common chemotherapy drug employed against breast, lung, and other cancers.
“This suggests a fundamental mechanism for enhancing myelination and maintaining oligodendrocyte integrity, regardless of the specific demyelinating agent, be it chemotherapy or another cause,” Tsai asserts.
Due to its broad potential, Tsai’s lab is currently exploring gamma treatment in mouse models for other neurological conditions, including Parkinson’s disease and multiple sclerosis. Cognito Therapeutics, a venture founded by Tsai and MIT Professor Edward Boyden, has recently completed a phase 2 trial of gamma therapy in Alzheimer’s patients and is gearing up for a phase 3 trial this year.
“While our main focus remains on Alzheimer’s, we aspire to test this approach in additional indications,” Tsai concludes.
This research received support from the JPB Foundation, the Ko Hahn Seed Fund, and the National Institutes of Health.
Photo credit & article inspired by: Massachusetts Institute of Technology