The effectiveness of a surgical patient’s pain management—referred to as “nociception”—often hinges on the anesthesiologist’s ability to assess and address unconscious pain. This is significant because it can greatly influence the patient’s experience of post-operative side effects and their need for pain relief. However, pain is inherently subjective, making it difficult to evaluate even when a patient is conscious, let alone when they are under anesthesia.
In an innovative study published in the Proceedings of the National Academy of Sciences, researchers from MIT and Massachusetts General Hospital (MGH) unveiled a series of statistical models designed to objectively quantify nociception during surgical procedures. Their goal is to assist anesthesiologists in optimizing medication dosages to reduce both post-operative pain and the associated side effects.
The study is based on extensive data gathered over 18,582 minutes from 101 abdominal surgeries at MGH, involving both male and female patients. Led by Sandya Subramanian, PhD ’21, currently an assistant professor at the University of California at Berkeley and the University of California at San Francisco, the research team analyzed data from five different physiological sensors to capture responses during 49,878 distinct nociceptive events, such as surgical incisions or cautery. In addition, they meticulously recorded all administered drugs, their dosages, and timing, allowing them to consider the effects of these medications on nociception and cardiovascular functions. The comprehensive data set enabled the development of statistical models capable of predicting the body’s response to nociceptive stimuli effectively.
The essence of this research is to provide anesthesiologists with precise and objective physiological data in real time, as they often rely on intuition and past experiences to guide drug administration for pain management during surgery. An inadequately administered dosage can lead to adverse side effects, such as nausea or delirium, while insufficient doses may result in unnecessary pain once the patient regains consciousness.
“Sandya’s work has advanced our understanding of nociception during general anesthesia,” stated study senior author Emery N. Brown, an Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience at MIT and an anesthesiologist at MGH, as well as a professor at Harvard Medical School. “Our next aim is to translate our findings into practical tools for anesthesiologists to implement during surgical procedures.”
Linking Surgery with Statistics
The groundwork for this research was laid during Subramanian’s doctoral thesis project in Brown’s lab in 2017. Previous efforts to quantitatively model nociception focused primarily on ECG (electrocardiogram), which only indirectly indicates heart-rate variability, or relied on other systems that either used superficial laboratory experiments or aggregated data from limited time points spread across different patients. “The surgical environment is the only place to accurately assess surgical pain,” Subramanian noted. “We aimed not only to develop algorithms based on actual surgical data but also to validate them in the very context where they will be applied.”
To enhance their capabilities, Subramanian and Brown gathered comprehensive multi-sensor data throughout actual surgeries while considering the influence of administered drugs. This approach was designed to yield a model that could produce reliable predictions tailored to each patient’s response throughout the procedure.
One of the notable advancements from this study involved tracking both heart rate patterns and skin conductance. Fluctuations in these physiological responses can signal the body’s inherent “fight or flight” reaction to pain. However, since certain anesthetic drugs can directly impact cardiovascular function, skin conductance (also known as electrodermal activity or EDA) is a stable measure unaffected by these interventions. The study utilized both ECG and PPG (photoplethysmography), an optical heart rate monitoring method, since ECG data can become distorted by the operating room’s numerous electrical devices. Similarly, EDA measures were corroborated with skin temperature readings to differentiate sweating from nociception against the backdrop of surgical conditions. Additionally, respiration was monitored.
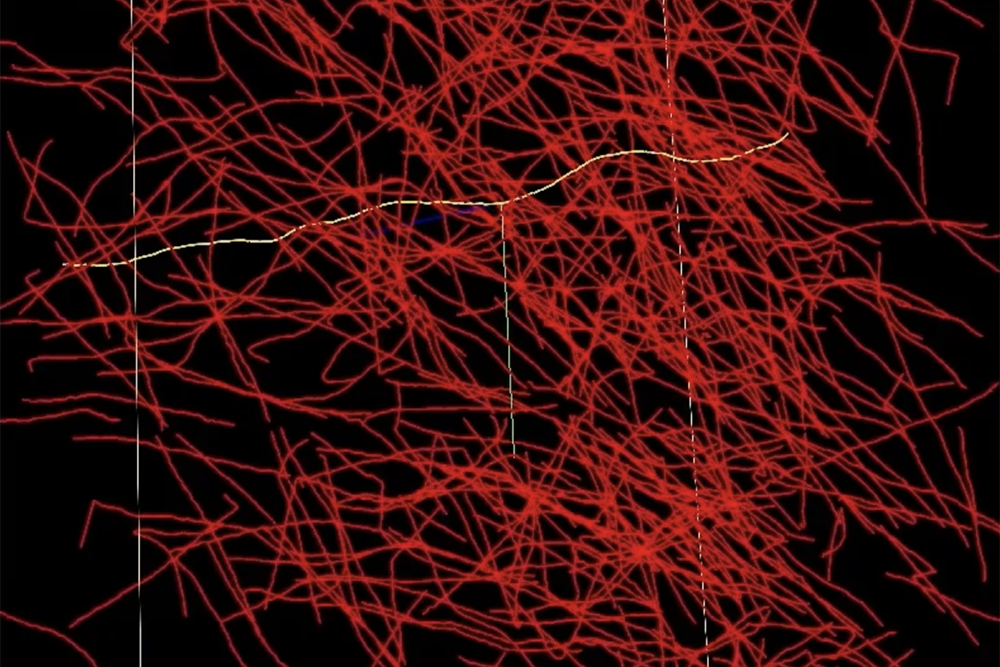
Next, the researchers conducted statistical analyses to derive relevant physiological indices from cardiovascular and skin conductance signals. They then synthesized these indices to create comprehensive models capable of predicting nociception and consequent bodily reactions.
Capturing Nociception Accurately
Subramanian honed multiple model versions, providing them specific inputs about when nociceptive stimuli occurred, allowing the models to correlate physiological data with pain-inducing events. Some models disregarded drug data, while others applied varied statistical methods, such as “linear regression” or “random forest.” A fifth model, leveraging a “state space” strategy, was left unsupervised to discern nociception from the physiological measurements alone. All models were evaluated against an established industry benchmark known as the ANI model.
The output from these models can be visualized as a time graph depicting the anticipated level of nociception. While the ANI model performed slightly above chance, the unsupervised model exceeded chance levels significantly, demonstrating the potential for detecting nociceptive states across a range of patients. The top-performing model incorporated drug information and employed the random forest technique, showcasing the complexity of physiological responses to surgical stimuli.
“Using a state space approach with multisensory physiological observations is effective in defining this implicit nociceptive state and provides a consistent interpretation across various subjects,” wrote Subramanian, Brown, and their colleagues. “This represents a critical advancement in creating metrics to monitor nociception without requiring primary nociceptive data.”
The next phase of this research will focus on enhancing data collection methods and refining the models for real-time application in the operating room. Successful integration of these predictive systems will empower anesthesiologists to make informed decisions about pain management strategies. In the long run, this could lead to the development of automated systems that adjust drug dosages under the anesthesiologist’s oversight.
“Our study marks a significant leap toward developing objective markers for surgical nociception,” the authors concluded. “These markers will facilitate objective assessments in complex clinical settings, such as ICUs, and propel the future design of automated pain management systems.”
Alongside Subramanian and Brown, the research team included Bryan Tseng, Marcela del Carmen, Annekathryn Goodman, Douglas Dahl, and Riccardo Barbieri.
This study received funding from various sources, including The JPB Foundation, The Picower Institute, and additional esteemed donors.
Photo credit & article inspired by: Massachusetts Institute of Technology