Imagine a future where diagnosing lung cancer is as straightforward as inhaling tiny nanoparticle sensors and simply providing a urine sample for testing. Thanks to groundbreaking technology developed at MIT, this vision may soon become a reality.
The innovative diagnostic method employs nanosensors that can be administered through an inhaler or nebulizer. When these sensors detect cancer-associated proteins in the lungs, they generate a signal that later accumulates in the urine, allowing for identification via a convenient paper test strip.
This new approach could serve as a replacement or complement to the current gold standard for lung cancer diagnosis: low-dose computed tomography (CT). Its impact could be especially profound in low- and middle-income countries, where access to CT scanners is often limited, according to the research team.
“Globally, cancer prevalence is rising, particularly in low- and middle-income countries. The driving factors for lung cancer there include pollution and smoking, making this technology an essential tool for enhancing accessibility,” states Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology and a member of MIT’s Koch Institute for Integrative Cancer Research.
Bhatia is the senior author of a study published in Science Advances, with Qian Zhong, an MIT research scientist, and Edward Tan, a former MIT postdoc, as the lead authors.
Revolutionary Inhalable Nanoparticles
In an effort to facilitate early lung cancer detection, the U.S. Preventive Services Task Force recommends annual CT scans for heavy smokers aged 50 and above. However, many in this demographic do not receive these screenings, and CT scans often have high false-positive rates, which can lead to unnecessary invasive procedures.
For the past decade, Bhatia has focused on creating nanosensors designed for cancer and disease diagnoses. This latest research explores the potential of these sensors as a more accessible alternative to traditional CT screenings for lung cancer.
These sensors are made from polymer nanoparticles that are coated with a reporter, like a DNA barcode. When the sensors come into contact with specific proteases—enzymes that are often elevated in tumors—they release the reporter, which later appears in urine.
Previous iterations of these sensors were designed for intravenous delivery targeting cancers in the liver and ovaries. The goal for lung cancer detection was to develop an inhalable version, simplifying deployment in under-resourced areas.
“Our objective was to create a diagnostic method that ensures high specificity and sensitivity while also enhancing accessibility, addressing disparities in early lung cancer detection,” says Zhong.
To accomplish this, the researchers formulated two types of their particles—a solution that can be aerosolized via a nebulizer, and a dry powder for inhalers.
Once inhaled, the particles are absorbed in the lung tissue, interacting with proteases that may be present. Normal human cells express a variety of proteases, many of which become overactive in tumors, facilitating cancer cells’ migration. These cancer-specific proteases cleave the DNA barcodes from the sensors, permitting their circulation in the bloodstream until they are excreted through urine.
In earlier iterations, mass spectrometry was utilized to analyze urine samples for DNA barcodes, but given the lack of mass spectrometry equipment in resource-limited settings, the researchers created a lateral flow assay. This allows for detection with a simple paper test strip.
The design of the strip enables it to detect up to four different DNA barcodes, each corresponding to a specific protease. No pre-treatment or complex processing of urine samples is needed; results can be read in just 20 minutes.
“We aimed to develop an assay that is point-of-care available in resource-limited environments, eliminating the need for sample processing or amplification, allowing for immediate reading of results,” Bhatia explains.
Promising Diagnostic Accuracy
The team evaluated their diagnostic method on genetically modified mice that develop lung tumors akin to those in humans. The sensors were introduced 7.5 weeks after tumor initiation—an equivalent timeframe for early-stage human cancer.
During initial experiments, they assessed 20 different sensors targeting various proteases. Using a machine-learning algorithm, the researchers identified an optimal combination of just four sensors capable of delivering accurate diagnoses. Upon testing this combination, they confirmed its effectiveness in early-stage lung tumor detection in mice.
For human applications, additional sensors may be necessary for accurate diagnosis, which could be facilitated by deploying multiple test strips, with each detecting different DNA barcodes.
The next steps involve analyzing human biopsy samples to verify the sensor panels’ effectiveness in detecting human cancers. Looking ahead, the researchers are eager to initiate clinical trials. Notably, a company named Sunbird Bio has already begun Phase 1 trials with a similar sensor from Bhatia’s lab for diagnosing liver cancer and nonalcoholic steatohepatitis (NASH).
In regions where CT scans are scarce, this innovative technology holds the potential to revolutionize lung cancer screening, significantly streamlining the diagnostic process.
“The vision is for individuals to receive immediate feedback regarding the necessity for follow-up tests, quickly ushering those with early-stage lesions into treatment pathways that could save lives or facilitate curative surgeries,” Bhatia shares.
This research received funding from various institutions, including the Johnson & Johnson Lung Cancer Initiative, Howard Hughes Medical Institute, and the National Cancer Institute, among others.
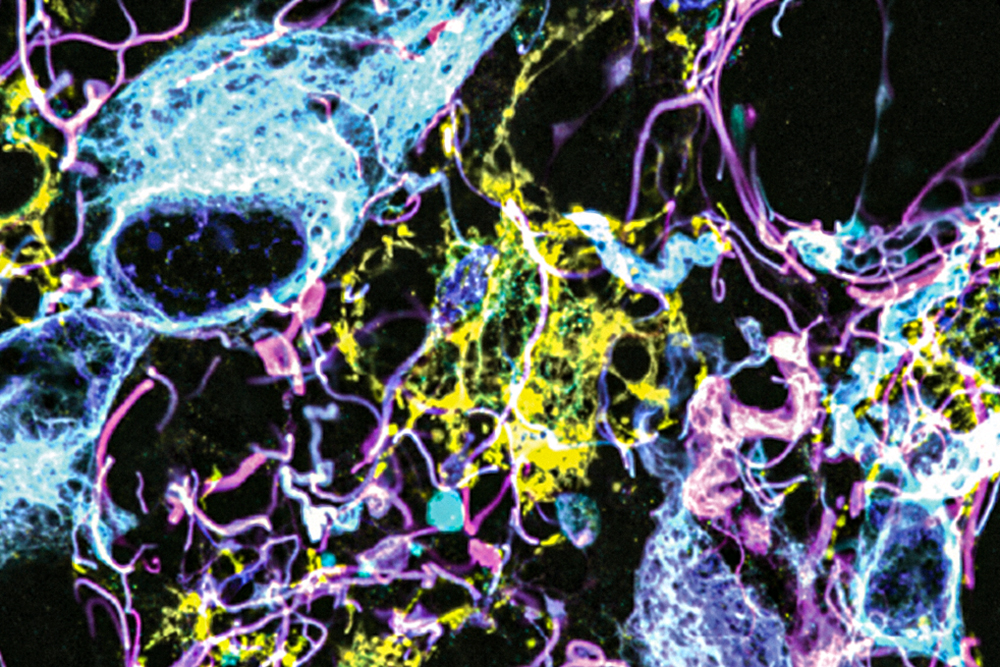
Photo credit & article inspired by: Massachusetts Institute of Technology