Anesthesiologists have a variety of drugs at their disposal to induce unconsciousness in patients, yet the intricate workings behind how these substances affect the brain have remained a mystery. Recent research conducted by neuroscientists at MIT has shed light on this subject, particularly focusing on the popular anesthetic drug propofol.
Through innovative methods to analyze neuron activity, the research team uncovered that propofol induces unconsciousness by upending the brain’s delicate equilibrium between stability and excitability. Essentially, the drug leads to a state of heightened instability in brain activity, which ultimately results in the loss of consciousness.
“The brain must function on a very fine line between being excitable and chaotic. It has to be responsive enough for neurons to communicate, but if it becomes overly excitable, it descends into chaos. What propofol does is disrupt the systems that maintain this critical balance,” explains Earl K. Miller, the Picower Professor of Neuroscience and a member of MIT’s Picower Institute for Learning and Memory.
The findings, published in Neuron, may enhance researchers’ ability to create better monitoring tools for patients undergoing general anesthesia.
Miller, along with Ila Fiete, a professor of brain and cognitive sciences and director of the K. Lisa Yang Integrative Computational Neuroscience Center (ICoN), led the study, which also featured contributions from MIT graduate student Adam Eisen and postdoctoral researcher Leo Kozachkov.
Understanding Unconsciousness
Propofol works by binding to GABA receptors, inhibiting the activity of neurons that carry these receptors. While various anesthetic drugs are known to act on different types of receptors, the exact processes through which these substances induce unconsciousness are not completely understood.
Miller, Fiete, and their team proposed that propofol—and potentially other anesthetic agents—disturb a brain state referred to as “dynamic stability.” In this condition, neurons maintain sufficient excitability to react to inputs while the brain adeptly regains control, preventing excessive excitement.
Conflicting studies have emerged regarding the effects of anesthetic drugs on this stability: some indicate that anesthesia leads the brain to become overly stable and unresponsive, while others suggest it becomes excessively excitable, spiraling into chaos, thus resulting in unconsciousness. These inconsistencies can, in part, be attributed to the challenges of accurately measuring dynamic stability during this process.
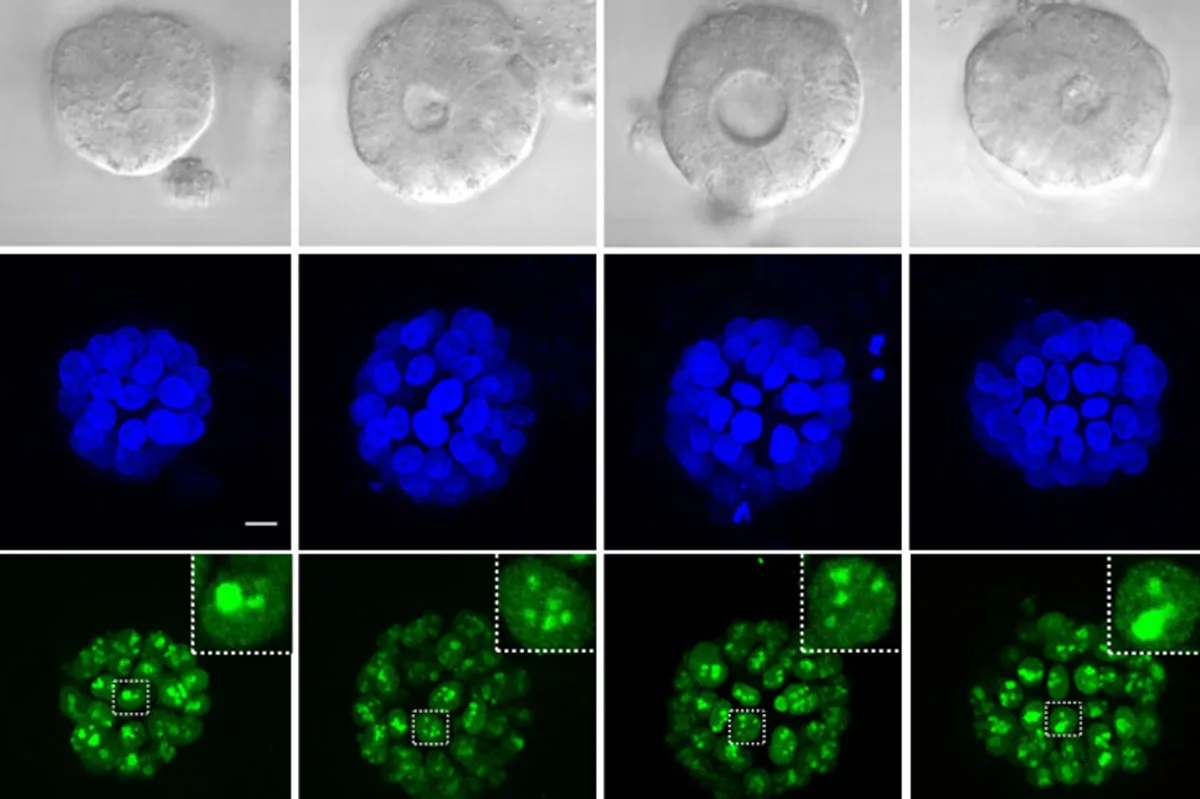
In their experiments, researchers observed electrical activity in the brains of animals over an hour as they received propofol and gradually lost consciousness. Measurements were taken in four key brain areas related to vision, auditory processing, spatial awareness, and executive function.
To capture a broader understanding of brain activity despite having limited recordings, the researchers employed a method known as delay embedding. This technique enhances the analysis of dynamic systems by incorporating previous measurements into the current data.
The researchers identified that in a normal waking state, neural activity spikes following sensory inputs and swiftly returns to its baseline. However, as propofol was administered, the time taken for the brain to revert to its baseline increased significantly, leading to prolonged periods of heightened excitement. This worsening effect continued until the subjects ultimately lost consciousness.
This suggests that propofol’s inhibition of neuronal activity creates a vicious cycle of increasing instability, culminating in the loss of consciousness.
Advancing Anesthesia Management
To further explore these findings, the team created a straightforward computational model of neural networks. When they simulated increased inhibition in specific network nodes—mirroring propofol’s impact in the brain—instability became evident in the network’s activities, resembling the disruptions observed in the actual subjects under propofol.
“We examined a basic circuit model of interconnected neurons, and by enhancing inhibition within that model, we noticed a similar destabilization. We’re proposing that increased inhibition leads to instability, which parallels the onset of unconsciousness,” states Eisen.
As Fiete elaborates, “This counterintuitive phenomenon, where heightened inhibition destabilizes rather than quiets the network, stems from disinhibition. When propofol amplifies inhibitory activity, it inadvertently inhibits other inhibitory neurons, leading to an overall surge in brain activity.”
The research team suspects that various anesthetic agents may trigger similar destabilizing effects through disparate mechanisms—a hypothesis they’re currently investigating.
If validated, this notion could significantly aid in developing methods for more precise control over anesthesia levels in patients. Collaborating with Emery Brown, the Edward Hood Taplin Professor of Medical Engineering at MIT, Miller is working on systems that continuously measure brain dynamics and adjust drug dosages in real-time.
“If we identify shared mechanisms across different anesthetics, we’ll be able to enhance their safety by fine-tuning a few parameters rather than establishing unique protocols for each anesthetic,” Miller emphasizes. “What we need is a unified system that addresses all anesthetic types used in the operating room.”
The researchers are also keen to apply their dynamic stability measurement technique to various brain states, including neuropsychiatric disorders.
“This methodology is potent, and I anticipate it’s going to be exciting to utilize it for examining different brain states, a variety of anesthetics, and conditions like depression and schizophrenia,” Fiete concludes.
The research was supported by multiple organizations, including the Office of Naval Research, the National Institute of Mental Health, and the National Institute of Neurological Disorders and Stroke, among others.
Photo credit & article inspired by: Massachusetts Institute of Technology