When medical devices like pacemakers are implanted, they often trigger an immune response that results in scar tissue formation around the device. This process, known as fibrosis, can hinder the device’s effectiveness and may necessitate its removal.
In a significant breakthrough aimed at combating this issue, engineers at MIT have developed a versatile approach to reduce fibrosis by applying a hydrogel adhesive coating on devices. This innovative adhesive promotes bonding to biological tissue, thereby shielding the implant from immune system attacks.
“Many research teams and companies aspire to create implants that the body accepts over time, enabling the device to perform its therapeutic or diagnostic role without complications. With this new ‘invisibility cloak,’ we are moving closer to that vision—requiring neither medication nor specialized polymers,” explains Xuanhe Zhao, MIT professor of mechanical engineering and civil and environmental engineering.
The hydrogel adhesive utilized in this research comprises cross-linked polymers and resembles a surgical tape previously developed by the team for internal wound sealing. The researchers discovered that different hydrogel types could also provide protection against fibrosis, suggesting this method’s potential application not only for pacemakers but also for sensors and drug delivery devices.
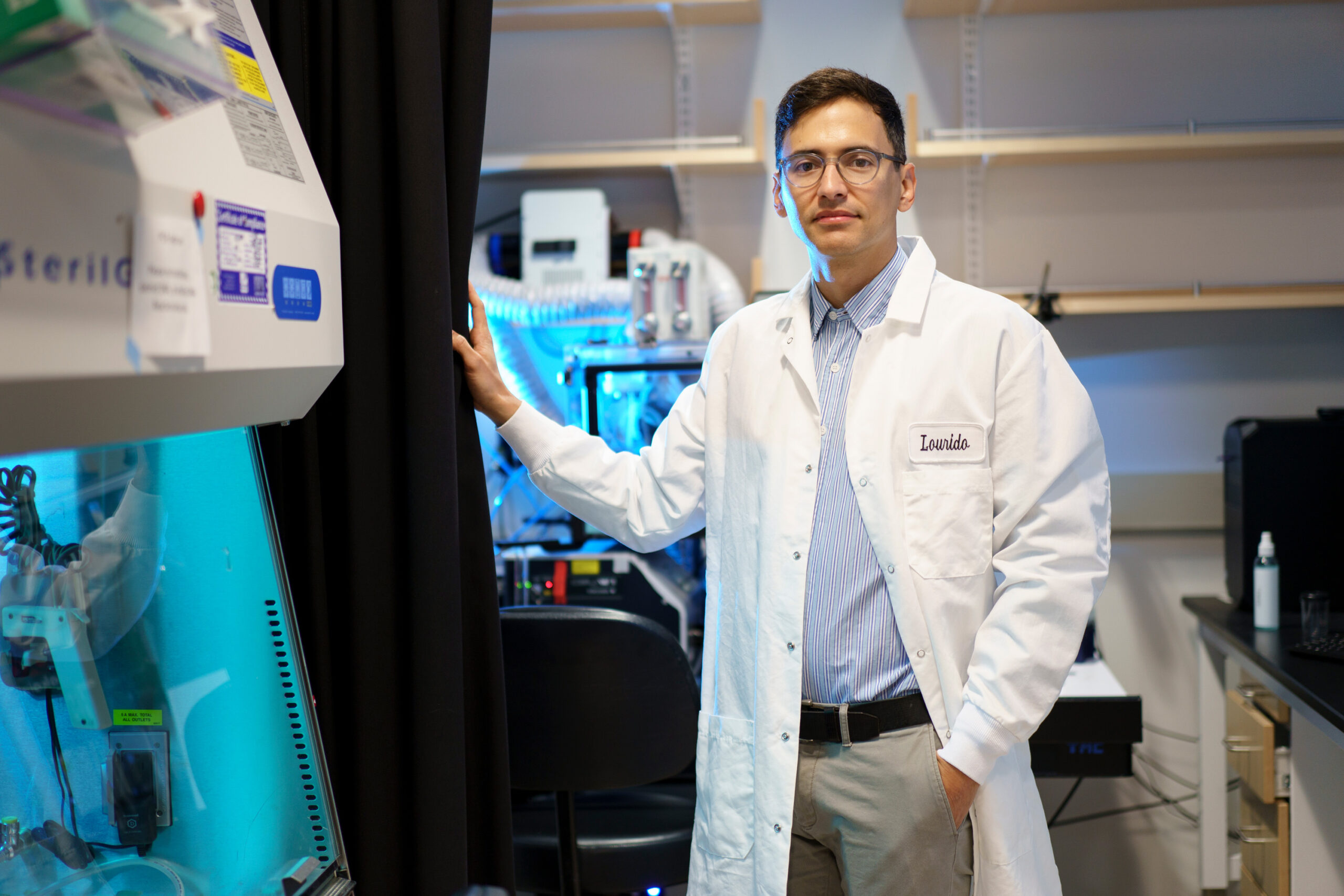
Zhao and Hyunwoo Yuk SM ’16, PhD ’21, the former MIT research scientist who is now the chief technology officer at SanaHeal, are the senior authors of a study that was published in Nature. Jingjing Wu, a postdoctoral researcher at MIT, served as the lead author.
Mitigating Fibrosis
Over recent years, Zhao’s lab has pioneered a variety of adhesives tailored for medical uses, including single-sided and double-sided tapes suitable for surgical incisions or internal injuries. These adhesives efficiently absorb water from moist tissues through polyacrylic acid, a material commonly found in diapers. This process enables strong chemical bonds with surface proteins within approximately five seconds.
Several years back, Zhao and Yuk began investigating whether this type of adhesive could ensure medical implants remain securely in place and minimize fibrosis.
To assess this hypothesis, Wu coated polyurethane devices with the adhesive and implanted them in various areas of rats, including the abdominal wall, colon, stomach, lungs, and heart. Weeks later, upon removal, there was no visible scar tissue. Testing in multiple animal models produced the same result: implanted adhesive-coated devices demonstrated no fibrosis for up to three months.
“This research reveals a broad strategy, applicable across various animal models, organs, and applications,” Wu affirmed. “Across all our tests, we consistently observed no fibrotic capsule formation.”
Employing bulk RNA sequencing and fluorescent imaging, the researchers evaluated the immune response and found that while immune cells like neutrophils infiltrated the area where the adhesive-coated devices were implanted, their presence quickly diminished before any scar tissue could develop.
“With the adhered devices, an acute inflammatory response occurs since they are foreign materials,” Yuk elaborated. “However, this inflammatory response significantly decreases over time, preventing fibrosis.”
This adhesive may find application in epicardial pacemakers, which are placed on the heart to manage heart rate. The research team discovered that adhesive-coated wires implanted in rats maintained functionality for at least three months without developing scar tissue.
“The formation of fibrotic tissue at the junction between implanted medical devices and surrounding tissue is a persistent issue that leads to device failure. Our demonstration that strong adhesion can eliminate this fibrotic tissue formation is an important finding with vast implications for the medical device industry,” commented David Mooney, a Harvard University professor of bioengineering who was not involved in the study.
Understanding Mechanical Cues
The team also evaluated a hydrogel adhesive containing chitosan, a naturally occurring polysaccharide, which also effectively eliminated fibrosis in animal trials. Conversely, two commercially available tissue adhesives failed to demonstrate this antifibrotic effect due to their eventual detachment from the tissue, allowing the immune system to resume its attacks.
In another experiment, the researchers coated implants in hydrogel adhesives, subsequently treating them to negate their adhesive properties while preserving their chemical structure. When implanted in the body, where they were held with sutures, fibrosis occurred. This implies that the mechanical interaction between the adhesive and the tissue plays a crucial role in preventing immune system attacks.
“Previous immunology research has predominantly focused on chemical interactions, but mechanics and physics are equally essential. We should explore these mechanical cues in the context of immune responses,” Zhao stated, indicating plans to further investigate how mechanical cues impact the immune system.
Yuk, Zhao, and others have founded a company named SanaHeal, actively working on advancing tissue adhesives for medical applications.
“We aim to share our findings with the community and ignite curiosity about their broader potential,” said Yuk. “The possibilities for interfacing with foreign or manmade materials within the body are vast, including implantable devices, drug reservoirs, and cell depots.”
This groundbreaking research received funding from the National Institutes of Health and the National Science Foundation.
Photo credit & article inspired by: Massachusetts Institute of Technology