Therapeutic cancer vaccines represent a cutting-edge approach to combating malignancies. The premise is simple: when patients receive injections of peptide antigens—protein fragments exclusive to tumor cells—their T cells become equipped to detect and target cancer cells showcasing those specific proteins. This strategy aims not only to eradicate tumors but also to curb their potential recurrence.
However, in reality, effective cancer vaccines have remained elusive despite years of intensive research.
“Significant strides have been made to enhance the efficacy of cancer vaccines,” comments Darrell Irvine, a professor at MIT with expertise in Biological Engineering and Materials Science. He is also a key member of the Koch Institute for Integrative Cancer Research at MIT. “Yet, even in preclinical models, these vaccines often elicit a muted immune response. When advanced to clinical trials, their effectiveness frequently diminishes.”
Encouragingly, advancements may now be on the horizon. A groundbreaking vaccine, developed by Irvine and his MIT colleagues and further refined by Elicio Therapeutics—a startup founded by Irvine to translate research into clinical solutions—has demonstrated promising results in ongoing clinical trials. Early Phase 1 data indicates that this vaccine might provide a viable treatment option for pancreatic and other forms of cancer.
Investigating the Challenge
Haipeng Liu, who joined Irvine’s lab nearly 15 years ago as a postdoctoral researcher, set out to unravel the reasons behind the disappointing performance of cancer vaccines. He identified a pivotal issue: peptide vaccines often fail to generate a robust immune response because they do not efficiently migrate to lymph nodes, where T cells, capable of learning to fight cancer, are concentrated.
Previous attempts to direct peptides to lymph nodes lacked precision. Despite utilizing nanoparticles or antibodies aimed at lymphatic immune cells, a significant number of vaccine peptides either ended up in incorrect cells or failed to reach the lymph nodes altogether.
This led Liu to ponder a fundamental question: If the vaccine peptides were not making it to the lymph nodes, where did they go? Through his research, Liu, who is now an associate professor at Wayne State University, made groundbreaking discoveries that refined peptide transport to lymph nodes, developing a vaccine that showcased unexpectedly strong immune responses in mice. This innovative vaccine is now in the capable hands of Elicio Therapeutics, with early clinical results indicating a similar strong immune response in human subjects.
Liu’s initial experiments involved administering peptide vaccines to mouse models. He quickly found that peptides injected into the skin or muscle would often leak into the bloodstream, leading to dilution and degradation rather than proper transport to the lymph nodes. In an attempt to secure the peptide vaccine, he encapsulated it within a micellar nanoparticle—composed of “amphiphilic” molecules whose hydrophilic heads shield the peptide payload. He tested two types: one designed to securely enclose the peptide and a control that didn’t. Despite the complexity of the locked micelles, the immune response was disappointingly weak. Liu felt defeated.
However, Irvine was optimistic; the more adaptive control micelles unexpectedly yielded the strongest immune response he had witnessed. Liu had uncovered a promising solution, albeit not the one he initially anticipated.
Creating the Vaccine
As Liu continued his work with micellar nanoparticles, he explored the biological aspects of lymph nodes. He learned that after tumor removal, surgeons utilize a blue dye to image lymph nodes for metastasis assessment. Surprisingly, despite its small size, the dye does not disperse into the bloodstream. Instead, it binds to albumin—the predominant protein found in blood and tissue fluids—and navigates efficiently to lymph nodes.
The amphiphilic molecules in Liu’s control group exhibited behavior similar to the imaging dye. Following injection, the loosely structured micelles were dismantled by albumin, which then propelled the peptide payload to its intended target.
Inspired by the imaging dye’s mechanism, the team developed a vaccine that leveraged lipid tails to secure peptide chains to albumin molecules directed at lymph nodes.
After assembling their innovative albumin-utilizing vaccine, they trialled it in mouse models for HIV, melanoma, and cervical cancer. Their 2014 study revealed that peptides modified to bind with albumin produced T cell responses that were five to ten times more potent compared to peptides alone.
Subsequent studies demonstrated the capacity for even greater immune responses. One significant study combined a cancer-targeted vaccine with CAR T cell therapy to elicit a dramatic increase in antitumor T cell populations. While CAR T therapy has seen success in treating blood cancers like leukemia, it has struggled with solid tumors due to local T cell suppression. The synergistic effect of the vaccine and CAR T led to the destruction of 60% of solid tumors in mice, while CAR T administration alone elicited minimal impact.
Transforming Research into Patient-Centric Solutions
By 2016, with robust laboratory results in hand, Irvine was prepared to transition the vaccine from academic research to clinical application, establishing Elicio Therapeutics. “We strived to set a high standard in the lab,” Irvine explained. “By leveraging albumin biology—which is consistent between mice and humans—we observed ten-, thirty-, and forty-fold superior responses in animal models compared to traditional vaccine approaches, which inspired optimism for patient outcomes.”
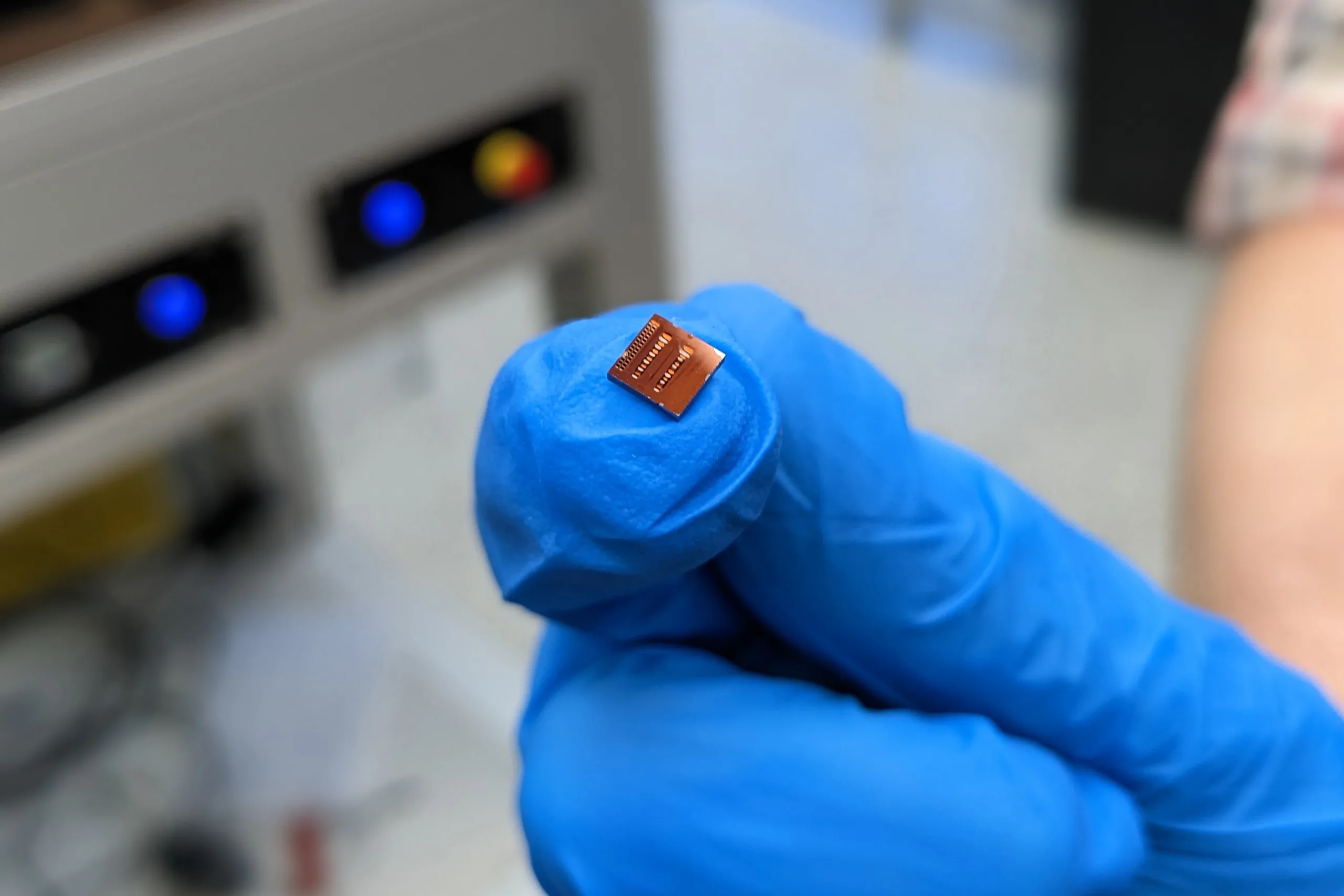
Today, Elicio’s vaccine has evolved into a platform that incorporates lipid-linked peptides along with an immune adjuvant—without requiring CAR T cells. In 2021, they launched a clinical trial, AMPLIFY-201, for a vaccine known as ELI-002, focused on cancers exhibiting mutations in the KRAS gene, specifically pancreatic ductal adenocarcinoma (PDAC). This vaccine addresses a critical need in cancer therapy, as PDAC is responsible for 90% of pancreatic cancer cases, noted for its aggressive nature and limited treatment options. Targeting KRAS mutations, which appear in 90-95% of PDAC instances, Elicio’s vaccine has the potential to approach seven KRAS variants simultaneously, which would cover 88% of PDAC cases. They have completed trials on a version targeting two variants, with ongoing Phase 1 and 2 studies on the broader seven KRAS mutant-targeting version.
Recent findings published in Nature Medicine highlight the promise of an effective therapeutic cancer vaccine. In the Phase 1 trial involving 25 patients (20 with pancreatic cancer and 5 with colorectal cancer), an astonishing 84% responded, showing an average 56-fold increase in antitumor T cells. Furthermore, blood biomarkers indicating residual tumors were completely eliminated in 24% of cases. Patients exhibiting robust immune responses saw an 86% reduction in cancer progression or mortality risk, with the vaccine proving well-tolerated and free from severe side effects.
“Joining Elicio has personal significance for me; my father battled KRAS-mutated colorectal cancer,” stated Christopher Haqq, Elicio’s executive vice president, head of research and development, and chief medical officer. “His experience underscored the pressing need for innovative treatments for KRAS-driven tumors, and I am hopeful that we are on a path to assist individuals like my dad and many others.”
Going forward, Elicio is currently testing the formulation of its vaccine targeting all seven KRAS mutations. Future plans also include addressing other KRAS-driven tumors, such as colorectal and non-small cell lung cancers. Peter DeMuth, PhD ’13, a former Irvine Lab graduate student and now Elicio’s chief scientific officer, believes that the collaborative research culture at the Koch Institute significantly influenced the vaccine’s evolution and the company’s vision.
“The approach at the Koch Institute, merging foundational science with engineering while fostering collaboration across diverse fields, was pivotal in shaping my perspective on innovation and my commitment to technology that can create tangible impact,” he reflected. “This unique ecosystem cultivated an engineering mindset alongside a thorough understanding of immunology, applied chemistry, and materials science—cornerstones of our work at Elicio.”
Funding for research pivotal to Elicio’s vaccine platform came, in part, from the Koch Institute Quinquennial Cancer Research Fellowship, the Marble Center for Cancer Nanomedicine, and the Bridge Project—a collaboration between the Koch Institute for Integrative Cancer Research at MIT and the Dana-Farber/Harvard Cancer Center.
This article was updated on Feb. 16 to clarify the ongoing clinical trial of the vaccine.
Photo credit & article inspired by: Massachusetts Institute of Technology