The opioid crisis continues to claim lives, with over 100,000 Americans succumbing to opioid overdoses in 2023. Quick intervention is crucial, and naloxone has proven to be the most effective antidote. However, timely access to this life-saving drug can often be a challenge, as first responders or bystanders may not always arrive in time.
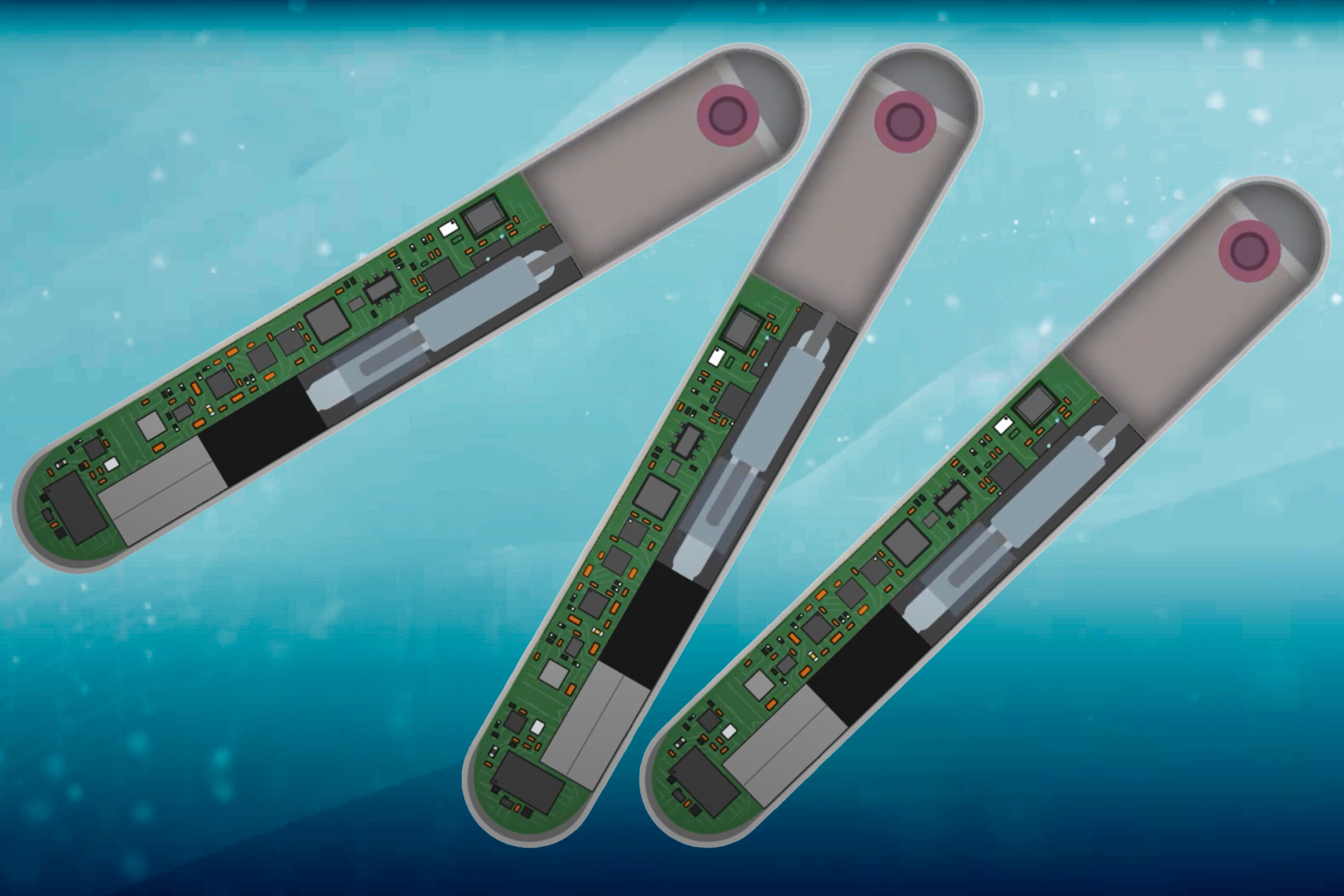
Combatting this pressing issue, researchers from MIT, in collaboration with Brigham and Women’s Hospital, have introduced a groundbreaking device designed to bridge these critical gaps. Roughly the size of a stick of gum, this innovative implantable device is designed to be placed under the skin to provide continuous monitoring of vital signs like heart rate and breathing. Upon detecting an overdose, it can rapidly administer naloxone, potentially saving lives.
In a recent study published in the journal Device, the researchers demonstrated that their device effectively reverses overdoses in animal models. As they advance their research, they envision this technology as a powerful tool to prevent opioid-related fatalities in high-risk populations, particularly among individuals who have previously experienced an overdose.
“This device addresses a significant unmet need within the substance abuse community to help mitigate the risk of fatal overdoses, focusing initially on those at high risk,” remarks Giovanni Traverso, an associate professor of mechanical engineering at MIT and a gastroenterologist at Brigham and Women’s Hospital.
The research team includes lead authors Hen-Wei Huang, now an assistant professor at Nanyang Technological University, and Peter Chai, an associate professor of emergency medicine at Brigham and Women’s Hospital, along with several other contributing scientists.
Understanding the Implantable Device
Naloxone is classified as an opioid antagonist, effectively binding to opioid receptors to block the effects of substances like heroin and fentanyl. Administered either through injection or nasal spray, naloxone can restore normal breathing within moments. Yet, many individuals who overdose do so in solitude, heightening the risk of fatality. The growing prevalence of synthetic opioids has further complicated matters, as overdoses can occur suddenly and unpredictably.
While some are exploring wearable devices equipped to detect overdoses, the MIT team has shifted focus to develop a less obtrusive solution—a miniaturized implant that can directly inject naloxone into the subcutaneous tissue. This innovative approach eliminates the need for patients to remember to wear a device.
The device includes advanced sensors capable of monitoring heart rate, breathing rate, blood pressure, and oxygen levels. Their studies on fentanyl overdoses helped create a specialized algorithm that enhances sensitivity, allowing the device to accurately identify an overdose event and differentiate it from other conditions, such as sleep apnea.
The research uncovered that fentanyl first induces a heart rate drop, quickly followed by a reduction in breathing. By closely monitoring these changes, the device can calculate the precise moment to trigger naloxone release.
“The most challenging part of creating this life-saving engineering solution is addressing patient adherence, combating stigma, minimizing false positives, and ensuring timely delivery of the antidote,” says Huang. “Our proposed approach innovatively use miniaturization, multi-sensing capabilities, continuous monitoring, and a novel micropumping mechanism.”
The implant houses a small reservoir capable of holding up to 10 milligrams of naloxone. Upon detecting an overdose, it activates a pump that delivers the drug within approximately 10 seconds.
In their experiments with animals, the researchers found that this method of administration reversed overdose effects in 96% of cases.
“We have created a closed-loop system that accurately senses the onset of an opioid overdose, releasing the antidote that leads to recovery,” states Traverso.
Paving the Path to Overdose Prevention
The vision for this technology is to assist individuals most susceptible to opioid overdoses, particularly those who have experienced them before. Future work will focus on enhancing user-friendliness and determining the optimal sites for device implantation.
“A crucial component in tackling the opioid crisis is to make naloxone readily available during critical moments of risk. We aim for this device to smoothly integrate into harm-reduction strategies, with the ultimate goal of preventing overdose deaths and supporting individuals dealing with opioid use disorders,” adds Chai.
The researchers aim to begin human trials within the next three to five years, while also working to further miniaturize the device and improve its on-board battery life, which currently lasts about two weeks.
The research has received funding from Novo Nordisk, the McGraw Family Foundation at Brigham and Women’s Hospital, and the MIT Department of Mechanical Engineering.
Photo credit & article inspired by: Massachusetts Institute of Technology