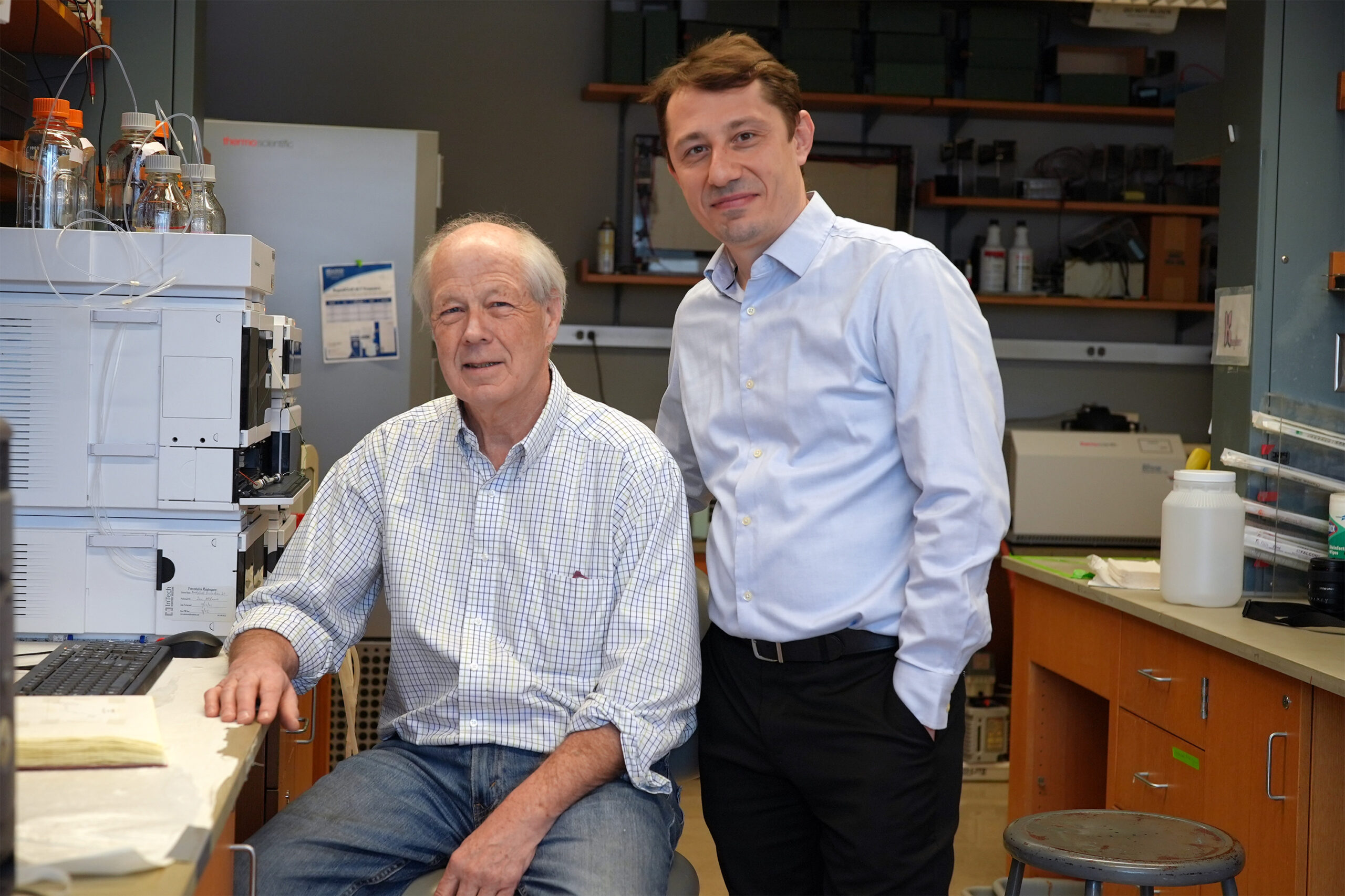
Associate Professor Thomas Heldt has been a vital part of the Massachusetts Institute of Technology (MIT) faculty since 2013, being a core member of the Institute for Medical Engineering and Science (IMES) and the Department of Electrical Engineering and Computer Science. In addition, Heldt plays a key role as a principal investigator at the Research Laboratory of Electronics (RLE) and leads the Integrative Neuromonitoring and Critical Care Informatics Group. Recently, he took on the role of associate director at IMES, focusing on internal affairs among other responsibilities.
Holding a PhD in Medical Engineering and Medical Physics (MEMP) from the Harvard-MIT Program in Health Sciences and Technology (HST) since 2004, Heldt’s research encompasses signal processing, estimation of physiological systems, mathematical modeling, and model identification aimed at improving real-time clinical decision-making, monitoring disease progression, and optimizing therapy in neurocritical and neonatal care settings. Here, he discusses his collaborative work with MIT colleagues and hospitals in the Boston area to leverage physiologic data for enhanced clinical outcomes.
Q: How does your research address clinical needs?
A: Our research examines the vast amounts of multimodal physiologic waveform data generated in critical, peri-operative, and emergency care environments. Currently, much of this information is typically evaluated visually by clinicians and discarded after just a few days, squandering the potential for systematic analysis and customised insights. To effectively analyze these data streams, we integrate a profound understanding of physiological processes over relevant time scales. This leads us to utilize reduced-order mathematical models that encapsulate the critical mechanisms necessary for clinical decision-making. For instance, we have successfully applied these techniques to estimate intracranial pressure non-invasively, make diagnostic decisions from capnogram shape analysis, and are now employing ultrasound methods to identify embolic events in patients with life support systems, such as ventricular assist devices or ECMO.
Q: Your collaborations with colleagues at MIT and clinicians in Boston are noteworthy. Can you share some impactful results from these partnerships?
A: Boston provides an incredible environment for translational research that connects our lab work at MIT with real patient populations! The collaborative and forward-thinking nature of our clinicians has been pivotal to our research and has provided invaluable mentorship for students and postdocs alike. We have gathered validation data from brain-injured patients in ICUs at several hospitals, including Boston Medical Center and Boston Children’s Hospital; this data helps us refine our capnography methods and our studies on embolic detection.
During our analysis at the neonatal ICU at BIDMC, we discovered that each baby was subject to an astonishing 177 alarms daily—one alarm approximately every eight minutes. This 54-bed neonatal ICU operates near capacity most days, and such noise heightens the risk of clinical staff becoming desensitized to alarms, potentially overlooking critical patient events. By scrutinizing alarm patterns and thresholds, we recommended changes to heart rate alarm thresholds, resulting in a 50% reduction in these alarms per patient daily. Following this adjustment, no adverse events were reported in the following months, leading the hospital safety committee to approve the changes permanently.
Furthermore, collaborating with the MGH Emergency Medicine Department, we developed a triage system to identify patients at risk for septic shock. With over 120,000 patients visiting the MGH emergency department yearly, timely identification of potential sepsis cases is critical. Our efforts significantly improved the speed of antibiotic administration for sepsis patients in the emergency department, subsequently validated across other Partners hospitals and incorporated into their electronic medical record system.
Q: Can you tell us about your background and what sparked your interest in systems physiology and biomedicine? What are your research ambitions and career objectives?
A: My journey began with a focus on physics in Germany, which eventually led me to apply my knowledge to physiology and medicine. I crafted my MD/PhD program, combining both disciplines, sparked by a transformative experience in congenital heart defect surgeries. Despite moving to the US for graduate studies at Yale, where I delved into nonlinear optics, I continually sought clinical relevance in my work. This ambition led me to the HST program, resulting in my long-standing career at MIT.
Currently, our research aims to innovate monitoring techniques for brain injury patients, with a focus on developing new, non-invasive algorithms and devices. These would replace conventional invasive monitoring methods and furnish actionable insights into brain physiology to guide therapeutic decisions. I aspire to see some of these techniques integrated into routine clinical practice.
At IMES and MIT, collaboration is a core value, and I eagerly anticipate working alongside colleagues to tackle significant challenges that none of us could manage alone—making it an enjoyable journey as we go!
Photo credit & article inspired by: Massachusetts Institute of Technology