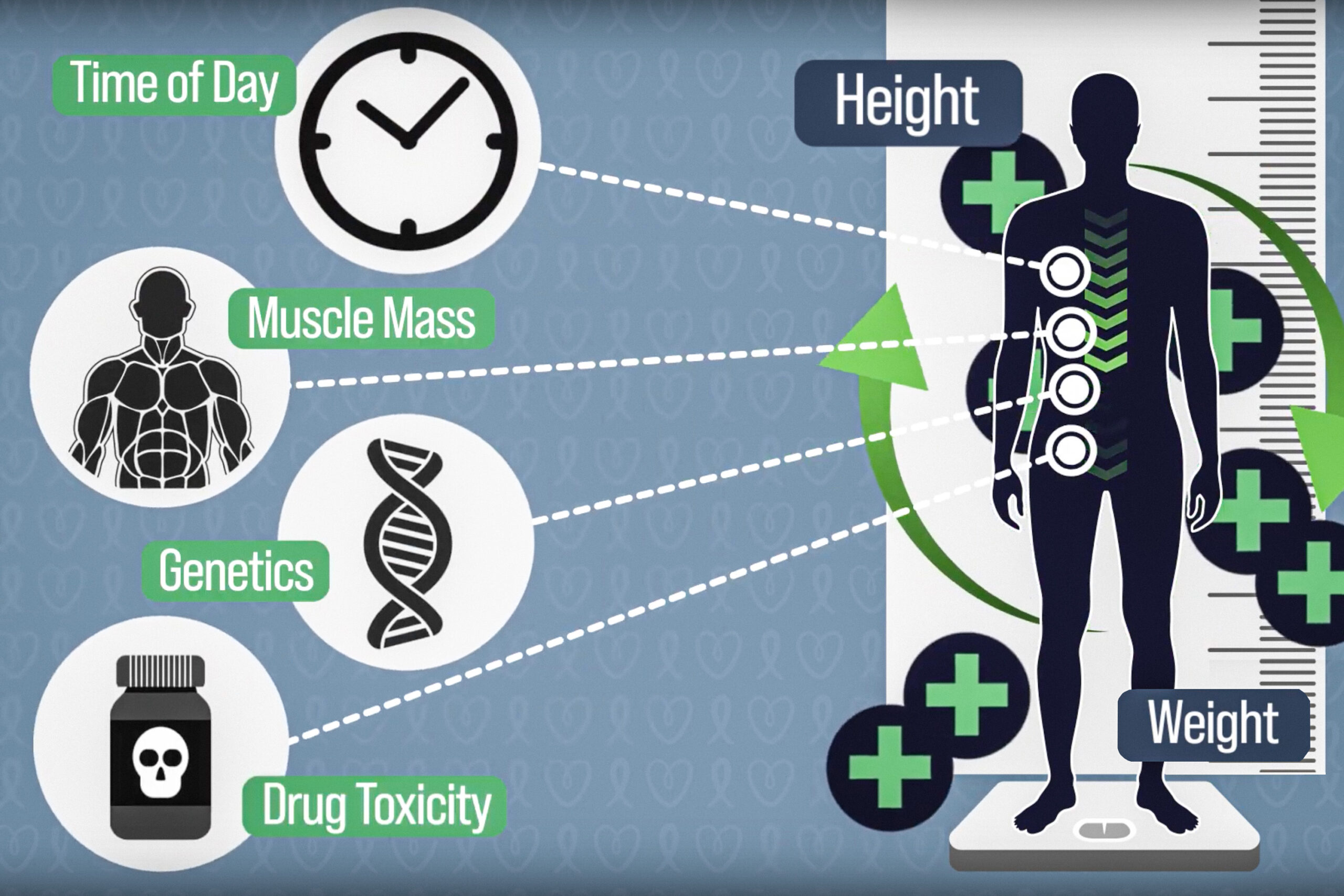
This groundbreaking system has the potential to address variances in drug pharmacokinetics influenced by various factors, including body composition, genetics, potential chemotherapy-induced organ toxicity, interactions with other medications or foods, and daily fluctuations in enzyme activity responsible for metabolizing these drugs. “By applying our enhanced understanding of drug metabolism alongside engineering techniques, we aim to revolutionize the safety and efficacy of numerous medications,” explains Giovanni Traverso, associate professor of mechanical engineering at MIT and a gastroenterologist at Brigham and Women’s Hospital, who is the senior author of the study.
The lead author, Louis DeRidder, a graduate student at MIT, highlights these findings in a recent study published in the journal Med.
Continuous Monitoring: A Game Changer
This research concentrated on 5-fluorouracil, a drug often used to treat colorectal cancer, typically administered over a 46-hour infusion. Traditionally, the dosage calculation is predicated on an equation derived from the patient’s height and weight, which merely estimates body surface area.
However, this method neglects essential differences in body composition and genetics, which can dramatically affect how the drug is distributed and metabolized. Such discrepancies can lead to severe side effects from overdosing or ineffective treatment from underdosing. “Individuals possessing the same calculated body surface area can variably experience significant differences in drug effects based solely on body composition,” notes DeRidder, a PhD candidate in the Medical Engineering and Medical Physics program of the Harvard-MIT Program in Health Sciences and Technology.
Another critical factor influencing drug levels in the bloodstream is the circadian rhythm of an enzyme named dihydropyrimidine dehydrogenase (DPD), which is responsible for metabolizing 5-fluorouracil. The expression of DPD, like many enzymes, fluctuates throughout the day. Consequently, DPD activity can dramatically alter the levels of 5-fluorouracil present in a patient’s body, leading to variations of up to tenfold during a single infusion period.
“Our current method, relying on body surface area, fails to address the wide variability in patient responses to 5-fluorouracil,” remarks Douglas Rubinson, a clinical oncologist at Dana-Farber Cancer Institute and study co-author. “This antiquated dosing fails to evolve with the patient’s changing metabolic response, resulting in preventable suffering.”
As a solution, therapeutic drug monitoring is one existing strategy where patients provide a blood sample at the conclusion of a treatment cycle. This sample is subsequently analyzed for drug concentration, allowing for dosage adjustments in the next cycle. Although this technique supports improved patient outcomes, it’s not commonly implemented for drugs like 5-fluorouracil.
Addressing this gap, the MIT team developed an automated, real-time monitoring method that adjusts chemotherapy dosing dynamically, resulting in optimal patient outcomes. Their “closed-loop” system permits continuous monitoring of drug concentrations, allowing for prompt adjustments in the infusion rate, in line with the patient’s pharmacokinetics and circadian fluctuations.
Dubbed CLAUDIA (Closed-Loop Automated Drug Infusion Regulator), this innovative system employs standard equipment for its operations. It gathers blood samples every five minutes, preparing them swiftly for analysis, measuring 5-fluorouracil concentrations relative to a predetermined target range. Any discrepancy prompts an algorithm to adjust the infusion rate, ensuring the drug levels remain within therapeutic limits.
“We’ve developed a system capable of consistently measuring drug concentration while adjusting the infusion rate to maintain the drug within its therapeutic range,” DeRidder asserts.
Rapid Adjustments for Better Outcomes
In animal trials, CLAUDIA maintained drug levels within target ranges approximately 45 percent of the time; in contrast, traditional dosing methods secured this same range only 13 percent of the time. Though the team’s focus in this study was on maintaining drug concentration rather than measuring treatment effectiveness, achieving suitable drug levels is generally believed to correlate with improved outcomes and reduced toxicity.
Moreover, CLAUDIA successfully regulated 5-fluorouracil levels even when a DPD inhibitor was introduced. Animals without real-time monitoring experienced up to an eightfold increase in drug concentration. For the initial demonstration, each process was performed manually using readily available equipment, but there are plans to automate these steps further, eliminating the need for human intervention.
The researchers utilized high-performance liquid chromatography mass spectrometry (HPLC-MS) for precise measurements, a technique adaptable for detecting various drugs. “We envision a future where CLAUDIA interplays seamlessly with various drugs that exhibit the necessary pharmacokinetic properties for detection via HPLC-MS, paving the way for personalized dosing across an array of medications,” DeRidder adds.
This research was supported by the National Science Foundation Graduate Research Fellowship Program, the MathWorks Fellowship, MIT’s Karl van Tassel Career Development Professorship, the MIT Department of Mechanical Engineering, and the Bridge Project—a collaboration between MIT’s Koch Institute for Integrative Cancer Research and the Dana-Farber/Harvard Cancer Center.
Other contributors to the research include Kyle A. Hare, Aaron Lopes, Josh Jenkins, Nina Fitzgerald, Emmeline MacPherson, Niora Fabian, Josh Morimoto, Jacqueline N. Chu, Ameya R. Kirtane, Wiam Madani, Keiko Ishida, Johannes L. P. Kuosmanen, Naomi Zecharias, Christopher M. Colangelo, Hen-Wei Huang, Makaya Chilekwa, Nikhil B. Lal, Shriya S. Srinivasan, Alison M. Hayward, Brian M. Wolpin, David Trumper, Troy Quast, and Robert Langer.
Photo credit & article inspired by: Massachusetts Institute of Technology