In critical care situations or during significant surgical procedures, patients can experience dangerously high or low blood pressure levels, leading to potential organ dysfunction. It’s not merely sufficient for healthcare teams to recognize that blood pressure readings are out of the ordinary. To effectively address these variations, clinicians require insights into the underlying causes of these fluctuations. A groundbreaking study from MIT introduces a sophisticated mathematical framework that provides real-time, accurate information necessary for clinicians to make informed decisions.
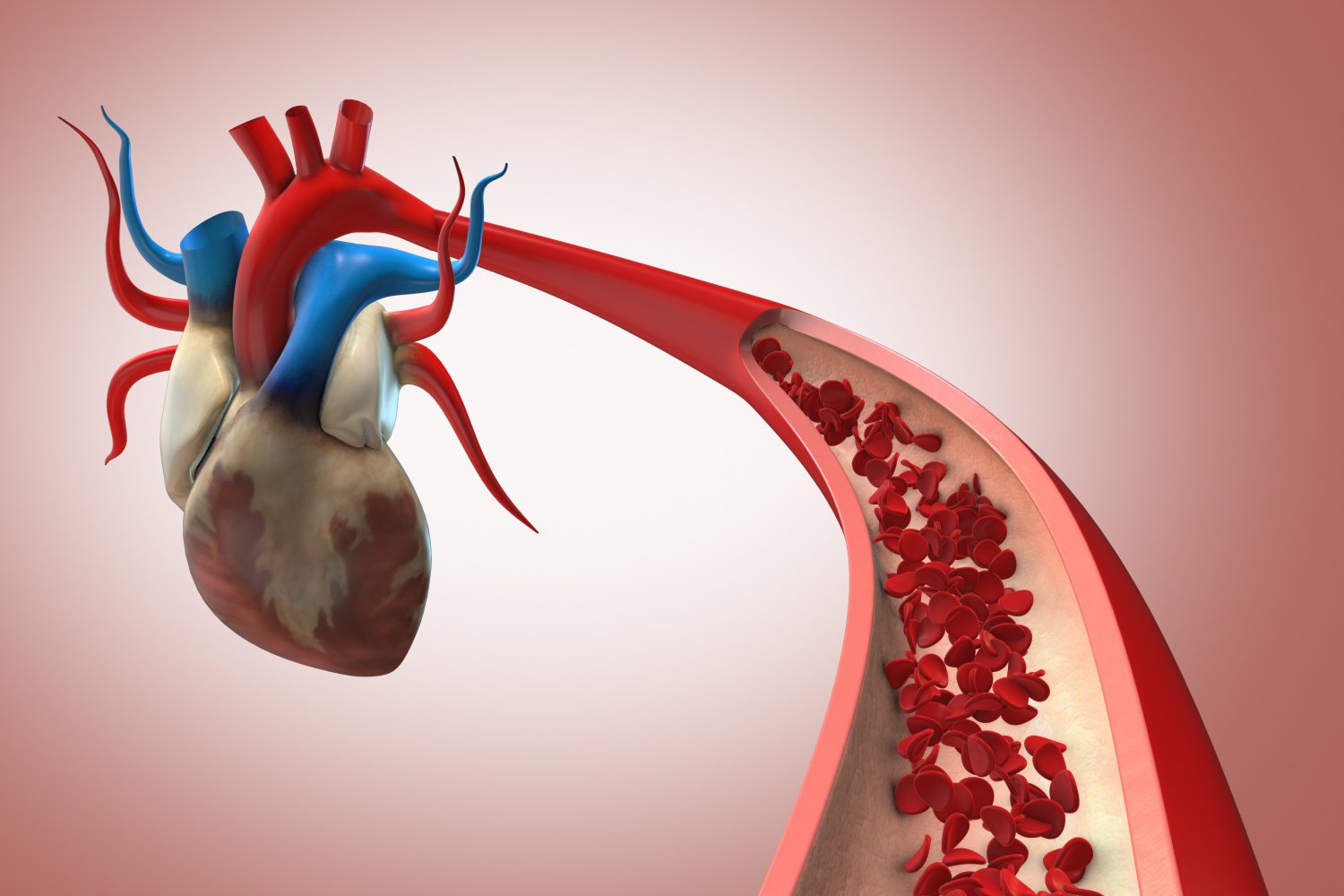
This innovative approach, detailed in a recent open-access study published in IEEE Transactions on Biomedical Engineering, offers proportional estimations of two key factors influencing blood pressure: the heart’s cardiac output (the volume of blood the heart pumps) and systemic vascular resistance (the resistance blood encounters as it flows through the circulatory system). By analyzing previously gathered data from animal models, the MIT researchers demonstrated that their findings, based on minimally invasive peripheral arterial blood pressure readings, align closely with the more invasive estimates derived from flow probes placed directly on the aorta. Additionally, they showed that their data effectively tracked changes when different medications were administered to adjust blood pressure.
“Our estimates for cardiac output and resistance can directly guide hemodynamic management in real time,” noted the authors of the study.
If further validation and regulatory approval are attained, this method could be transformative for heart surgeries, liver transplants, intensive care unit procedures, and a variety of other interventions influencing cardiovascular health.
“Any patient undergoing cardiac surgery might benefit from this technique,” said study senior author Emery N. Brown, who holds the Edward Hood Taplin Professorship in Medical Engineering and Computational Neuroscience at MIT. He is also an anesthesiologist at Massachusetts General Hospital and a professor of anesthesiology at Harvard Medical School. “Patients with compromised cardiovascular systems, like those suffering from ischemic heart disease, also stand to gain from stable blood pressure management.”
Leading this research was electrical engineering and computer science graduate student Taylor Baum, who collaborated closely with Brown and Munther Dahleh, the William A. Coolidge Professor in EECS.
Revolutionary Algorithm
The foundation of this study lies in the established Windkessel model, which posits that cardiac output and systemic resistance are pivotal to understanding blood pressure. However, prior methods attempting to apply this model encountered a dilemma: balancing the speed of estimate updates with their accuracy. This new MIT approach, under Baum’s leadership, leverages statistical and signal processing techniques such as state-space modeling to overcome these limitations.
“Our beat-by-beat estimates utilize not only data from the current heartbeat but also draw on historical data,” Baum explained. “This integration of past and present observations leads to more reliable estimates, updated continuously.”
Importantly, the method provides “proportional” estimates of cardiac output and systemic resistance, indicating an intrinsic mathematical relationship rather than treating them in isolation. Its application to earlier studies demonstrated that minimally invasive catheter readings from peripheral arteries like the leg or arm can yield insights on cardiovascular management comparable to those from traditional, more invasive aortic catheters.
Another significant discovery was that the proportional estimates reliably reflected physiological changes when animals were administered drugs to modify systemic vascular resistance or cardiac output, validating the method’s effectiveness.
From Research to Clinical Application
With these promising results, Baum and Brown are focused on seamlessly implementing this estimation method into clinical environments, intending to inform perioperative care teams about critical blood pressure changes. They are actively working towards obtaining regulatory approval for clinical device applications.
In addition, the researchers plan to continue animal studies for further validating this enhanced blood pressure management approach, and they have developed a closed-loop system that employs this estimation framework to precisely regulate blood pressure in animal models. Once these studies conclude, they will seek regulatory clearance to start human trials.
Alongside Baum, Dahleh, and Brown, the study’s authors include Elie Adam, Christian Guay, Gabriel Schamberg, Mohammadreza Kazemi, and Thomas Heldt. The research received support from the National Science Foundation, the National Institutes of Health, a Mathworks Fellowship, The Picower Institute for Learning and Memory, and The JPB Foundation.
Photo credit & article inspired by: Massachusetts Institute of Technology